Introduction
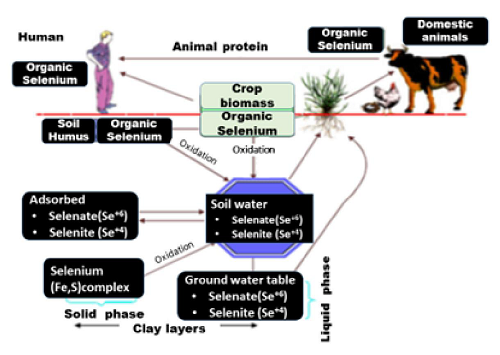
Selenium was first identified in 1817 by the Swedish chemist, Jons Jakob Berzelius. Selenium (Se) is a naturally occurring metalloid element that is called as the essential poison—too much of it in the diet can be toxic; too little can result in chronic, and sometimes fatal, deficiency. In the mid-19th century this syndrome was called alkali disease in South Dakota (USA) (Fordyce, 2005). Selenium is a bio accumulator which means that plants and animals retain the element in greater concentrations than are present in the environment and the element can be bio-concentrated by 200-6000 times.
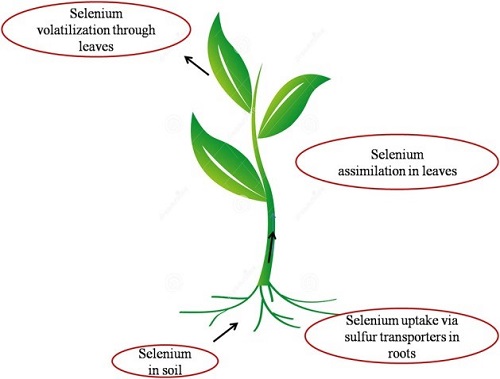
Selenium in Plants
Selenium is readily absorbed by all members of the plant kingdom (Anderson and others, 1961). Plants, even of the same species, may differ in their selenium concentration because of differences in available soil selenium. Interfering anions at the soil-root interface, root absorption. Translocation from roots to tops and dilution in the plant tops.
Plants have been divided into three groups: based upon their selenium-accumulating ability (National Research Council, 1976).
- Primary selenium-accumulator or indicator plants: may contain up to several thousand parts per million selenium. This group includes species of the genera Astragalus, Machaeranthera (section Xylorrhiia), Haplopappus (section Oonopsis), and Stardeya. Selenium accumulated by these plants is largely water soluble and in the form of low molecular weight organic compounds and selenate (National Research Council, 1983). The selenium is not incorporated into protein.
- Secondary selenium absorbers: may contain up to several hundred parts per million selenium, but lesser amounts are much more common. This group includes species of the genera Aster, Atriplex. Castilleja, Comandra, Gyria, Grindelia and Gutierrezia.
- The non-accumulator group: includes grasses, small grains, and alfalfa. Selenium absorbed by these plants is metabolized into plant proteins. These plants rarely accumulate more than 50 ppm selenium and usually only 5-12 ppm. The majority of selenium intoxications probably result from the grazing of plants in this category.
The toxicity of selenium-accumulating plants cannot be evaluated solely on the basis of the total selenium concentration. Various selenium compounds are likely to exhibit different intensities of toxicosis to animals. Also, plants, such as Astragalus and Happlopappus, contain other non-seleniferous constituents that may be toxic to animals.
Selenium Characterization
Selenium is quite unique as trace element, because it is a component of an amino acid, selenocysteine, typical of selenoproteins and therefore involved in very specific biological roles. Enzymes depending on selenium perform very important roles in the cells (Rayman 2000). The main roles are in protection against oxidative damages, defenses against infection, and modulation of growth and development. The main exposure to selenium occurs through food, and its distribution in the natural environment has a marked effect on its content in soils, crops, and the human body. Many of these effects can be linked to roles of the selenoproteins, and especially of glutathione peroxidases active as antioxidants and cell protecting agents. Deficiency of selenium in the diet causes diseases in animals which often are endemic to specific regions.

Selenium in Livestock
Selenium has long been recognized as a mineral toxic to animals, but only recently has it been shown to be a nutritional requirement. Selenium was reported essential for animal health in 1957, nearly three decades after its implication with alkali disease and animal death (Schwartz and Foltz, 1957).
Se concentrations in the diets of different livestock classes.
| Species | Se Requirements (mg/kg diet) |
Species | Se Requirements (mg/kg diet) |
| Beef Cattle | 0.10 | Horses | 0.10 |
| Dairy Cattle | 0.30 | Immature Laying Chickens | 0.10-0.15 |
| Sheep | 0.10-0.20 | Laying Hens | 0.05-0.08 |
| Growing Pigs | 0.15-0.30 | Broiler Chicks | 0.15 |
| Gestating and Lactating Sows | 0.15 |
Selenium Deficiency
- Selenium deficiency has been implicated in retained placenta in cattle, persistent diarrhea in young calves, and white muscle disease in young calves and lambs.
- Deficiency can cause exudative diathesis, nutritional muscular dystrophy, and nutritional pancreatic dystrophy in
- Hepatoses dietetica, mulberry heart disease, nutritional muscular dystrophy, and infertility may occur in ewes not receiving enough selenium.
- Selenium concentrations required in the diet range from 0.05 to 0.10 ppm depending on availability to the animal. Dietary sulfur has been shown to compete with selenium absorption, both by the plant and the animal.
Selenium Intoxication
The classification of selenium intoxications in livestock as follows: Acute intoxication, chronic intoxication, Alkali disease, Blind staggers.
Acute Selenium Poisoning in animals
Acute selenium poisoning often results from short term foraging of highly seleniferous plants such as the indicator plants (Rosenfeld and Beath, 1964). This occurs when animals are very hungry and ingest seleniferous plants of low palatability but with high levels of selenium.
Acute poisoning
| Species | Minimum lethal dose of se in Selenate or Selenite form (mg/kg diet) |
| Cattle | 8.0-10.0 |
| Sheep | 8.0-10.0 |
| Horse | 3.30 |
| Pig | 17.0 |
| Dog | 4.0 |
| Cat, rabbit, rat | 1.5-3.0 |
Poisoning occurs in cattle, horses and swine. The symptoms is characterized by an abnormal posture, unsteady gait, diarrhea, abdominal pain, increased pulse and respiratory rate and death. In sheep signs have shown depression and sudden death. Cattle fed a high dose of seleniferous Astragalus plants over several days quite suddenly started bellowing with a high-pitched voice as if distressed, became excited, increased their respiratory rate became prostrate and died. Swine fed a selenium deficient diet are later more susceptible to acute intoxication than normal pigs. Gross pathological changes include petechial hemorrhages in the endocardium, acute congestion and diffuse hemorrhages in the lungs, enteritis and passive congestion in the liver. Acute congestion of the endocardium occurs. The lungs shows congestion and hemorrhaging in the alveoli. The mucosa of the stomach and intestine manifest edema, hemorrhage, and necrosis. The signs of poisoning in sheep are primarily increased respiration and sudden death.
Chronic Intoxication
Chronic selenium poisoning has been divided into two syndromes: Alkali disease and blind staggers
| Species | Minimum lethal dose of Se in Selenate or Selenite form (mg/kg diet) |
| Cattle | 5.0-50.0 |
| Sheep | 10.0 |
| Poultry | 15.0 |
| Pig | 7.0 |
Alkali disease
This has been reported in cattle, swine, and horses. This disease is associated with the consumption of seleniferous forages like hay, grain, grasses and palatable forbs for days weeks or even months. In these forages the selenium is largely incorporated into the protein and is not water soluble.
Chronic poisoning
Blind staggers
This has been shown in cattle and sheep and is associated with the consumption or selenium indicator plants over days or weeks.
Alkali Disease
Alkali disease may be the principle chronic manifestation of selenium poisoning. This disease results from the consumption of seleniferous grasses and grains that contain 5-40 ppm selenium. The forage is usually consumed over a period of weeks or more. Alkali disease has been produced by feeding inorganic sodium selenate and sodium selenite. Alkali disease is characterized by dullness, lack of vitality, emaciation, rough hair coat, loss of hair (especially the long hair of mane or tail) and lameness. Reduced fertility and reproductive performance occurs, especially in sheep and cattle. Other lesions may include liver cirrhosis, ascites, and myocardial necrosis/scarring.
Blind Staggers
Blind staggers results from grazing moderate amounts or indicator plants over a period of days or weeks. Selenium in these plants is readily extractable in water. Blind staggers has been observed in cattle and sheep but not in horses, swine and poultry.
In cattle, blind staggers appears in three stages:
In phase -1: The animal may demonstrate impaired vision, disregards objects in its path and stumbles over them or walks into them. The body temperature and respiration are normal but the animal has little interest in eating or drinking.
In phase -2: The clinical signs shows front legs weaken, failing to support the animal and animal becomes anorectic.
In phase- 3: The tongue and mechanism for swallowing become partially or totally paralyzed. The animal is nearly blind. Respiration becomes labored and rapid. Abdominal pain is apparent. The body temperature drops below normal. The cornea becomes cloudy and death may come suddenly. The animal dies of respiratory failure. A loss of weight occurs during the process so the animal appears emaciated. Recovery only occurs during phases 1 and 2. Microscopic changes include necrosis and cirrhosis of the liver, nephritis and impaction of the digestive tract.
In India, Se poisoning in cattle may arise within 10-42 days of feeding rice straw, leucerne or berseem with selenium levels 0.50-6.7mg/kg DM and soil have selenium levels 1.0-10.5mg/kg DM (Arora 1975, 1985).
Mitigation Measures for Selenium Deficiency and Toxicity
The foremost approach to preventing selenium related health disorders is determining the prevalence of selenium in the environment. This may require soil and forage analysis if such information has not been determined previously. Farmers can be trained to identify Se accumulator plants so that their animals can be moved to safer areas. In Se deficient areas supplementing selenium will be necessary. In areas where Se levels are high in the soils and forages, it is necessary to avoid pastures high in Se or adopt measures to counter the toxic effect of selenium.
In general, selenium deficiencies in animals are corrected by giving injections, dietary supplements, salt licks and drenches. While correcting selenium deficiencies, administration of organic selenium such as selenium methionine was found to result in higher tissue, serum, and whole blood selenium concentrations than by the administration of equivalent doses of selenite (Tiwari et al., 2006).
The level of dietary selenium needed to prevent deficiency depends on the vitamin E status and species of the host. Assuming normal vitamin E status of the animal, concentrations of 0.04 – 0.1 mg/kg (dry weight) of selenium in feedstuffs are generally adequate for most animals with a range of 0.15-0.20 mg/kg for poultry and 0.03-0.05 mg/k for ruminants and pigs (WHO, 1987). International standards for Se requirements for cattle are in the range of 0.1 to 0.18 mg/kg dry matter. Although there are no specific treatments to correct selenium toxicities in animals, recognition of seleniferous plants, proper land management and selective grazing may help prevent selenosis. Animals having a blood selenium level >1.5 µg/ml is indicative of impending selenium toxicosis and such animals should receive corrective measures to alleviate Se toxicity. Administration of reduced glutathione (GSH) intravenously at 5 mg/kg of BW reportedly arrested the toxic signs, prevented mortality and lowered glutathione peroxidase (GSH-Px) activity (Deore et al., 2005).
Se toxicity in buffaloes was reportedly treated successfully in India by Arora et al (1975) and Arora (1985), using a daily oral dose of a trace mineral mixture consisting of five sulfates (1 kg magnesium sulfate, 166 gm ferrous sulfate, 24 gm copper sulfate, 75 gm zinc sulfate and 15 gm cobalt sulfate). A daily dose of 30 gm of this Penta-sulfate per adult animal was given until recovery was noted (21-50 days).
References
- Ammerman C. B. and S. M. Miller. (1975) Selenium in ruminant nutrition. J. Dairy Sci. 58:1561-1577
- Arora, S. P. (1985) Livestock problems related to geochemistry in India including selenium toxicity and goiter. In: Proceedings of the First International Symposium on Geochemistry and Health, London, pp. 164-180.
- Arora, S. P., Kaur, P., Khirwar, S. S., Chopra, R. C. and R. S. Ludri. (1975) Selenium levels in fodders and its relationship with Degnala Disease. In. J. Dairy Sci. 28: 249-253
- Burau, R.G. (1985) Environmental chemistry of selenium. Calif. Agric. 39: 16-18
- Deore, M. D., Srivastava, A. K. and S.K. Sharma. (2005)Effect of reduced glutathione treatment on selenosis, blood selenium concentration and glutathione peroxidase activity after repeated short term selenium exposure in buffalo calves. Toxicology. 213: 169-174
- Fordyce, F. (2005) Selenium deficiency and toxicity in the environment. Ambio. 36:94–97
- Gupta, M., and S. Gupta. (2017) An Overview of Selenium Uptake, Metabolism, and Toxicity in Plants. Front. Plant Sci. 7: 2074
- Hasanuzzaman, M., M.A. Hossain, and M. Fujita. (2010) Selenium in higher plants: Physiological role, antioxidant metabolism and abiotic stress tolerance .J Plant Sci, 5: 354-375
- Mayland, H.F. (1994) Selenium in plant and animal nutrition. In: W.T. Jr. Frankenberger and S. Benson (eds.), Selenium in the Environment. Marcel Dekker Inc., New York, pp. 29-45
- Rayman, M.,P. (2000) The importance of selenium to human health. Lancet. 356: 233–241
- Rogers, P., A.,M. (1990) Selenium toxicity in farm animals: Treatment and prevention. Irish Vet J.43:151-153
- Scharz, K., Foltz, C.,M. (1957) Selenium as an integral part of Factor 3 against dietary necrotic liver degeneration. J Am Chem Soc. 79:3292–3293
- Tiwary, A. K., Stegelmeier, B. L., Panter, K. E., James, L. F. and J. O. Hall. (2006) Comparative toxicosis of sodium selenite and selenomethionine in lambs. J. Vet. Diagn. Invest. 18: 61-70
- WHO (1987) Environmental Health Criteria 58—Selenium. Geneva: WHO
- Wood, M. (2000) Kenaf and Canola-Selenium slurpers. USDA, Agricultural Research Service, June issue
- Yadav, S. K., Singh, I., Singh, D. and S. D. Han. (2005) Selenium status in soil of northern districts of India. J. En. Management. 75: 129-132





Be the first to comment