Introduction
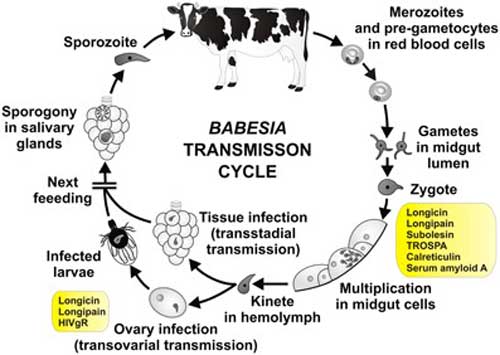
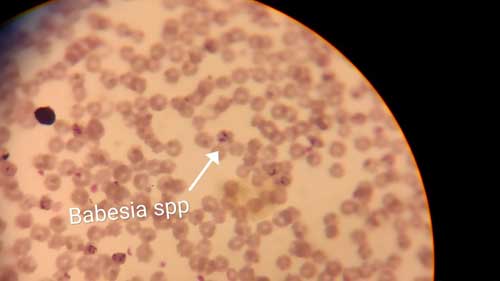
Babesiosis is tick born highly prevalent haemoprotozoal disease affecting cross breed as well as indigenous cattle in India. The principle strains are Babesia bovis & Babesia bigemina,with Rhicephalus ticks being the major vector. Morbidity & mortality vary with various factors like previous exposure to parasite, early diagnosis & treatment. The parasite comes under phylum Apicomplexa, order Piroplasmida and genus Babesia and species are Babesia bovis, Babesia bigeminia, Babesia divergens, Babesia major, Babesia ovata Babesia occultans etc. This organism mainly transmitted through tick as a vector. Babesia bovis, Babesia bigeminia transmitted through a Rhipicephalus spp. and Babesia divergens transmitted by Ixodes ricinus. Babesia parasites causes both acute and persistent subclinical disease in cattle.Babesia bovis is small parasite located centrally on the Red blood cell. Babesia bigemina typically pear shaped found in pairs in acute angle but Babesia bovis and Babesia divergens always found single on RBC.
Epidemiology
Babesiosis occurs throughout the world. The disease wide spread in Tropical and Sub-Tropical areas due to vector Boophilus microphilus. Bos indicus animals are resistant to disease compared to Bos torus. In summer occurrence will be in peak due high population of ticks.
Economic importance
This disease causing severe economical losses by affecting the productive animal’s performance in terms of milk and meat including deaths in acute cases. The disease is severe in young cattle leading to more deaths causing direct loss. Indirect losses are due to control of ticks and treatment cost of animal.
Zoonotic importance
This disease is having major zoonotic potential, tick bites are the source of infection.
Clinical signs
Incubation period will be 7-10 days. High fever, weakness, ataxia and in-coordination, dark or brown colour urine, anorexia, dullness , depression, fall in milk yield, pale to icteric conjunctival mucous membrane anemia and haemoglobinuria, cessation of rumination, labored breathing, accelerated heart rates and respiratory rates. General circulatory shock Sometimes nervous signs also shown and there will be loss of draft power in bullocks during pathogenesis phase of Babesiosis. Due to high fever pregnant animals will abort.

Post mortem lesions
Thin and watery blood may appear and Intravascular hemolytic condition. Pale icteric mucous membrane, icteric appearance of subcutaneous tissues, abdominal fat and omentum.Swollen liver with enlarged gall bladder with granular bile. Enlarged dark friable spleen. Enlarged yellowish Liver, Petechial hemorrhages and darker the kidneys. Bladder may contain red colour urine. Petechiae or ecchymoses on surface of heart brain, generalized anemia and jaundice. Edematous and hemorrhagic lymph nodes.
Diagnosis
- Based on clinical signs like High fever, passing coffee decoction colored urine and severe fall down in milk yield and presence of ticks.
- Sample such as blood and urine sample mainly collected for diagnosis of babesiosis.
- Microscopic examination of thick blood smear: The thick blood smear made and stained with Giemsa’s stain and observed under 100x oil immersion under microscope. This is traditional method for identification of parasite in the red blood cells. Pyriform organism observed in red blood cells.
- Nucleic acid-based diagnostic assay: this is PCR based diagnostic technique mainly used to identify the Babesia bovis, Babesia bigemini in carrier cattle. And it is used as most of the time conformation diagnostic tool for babesiosis.
- Occult blood test positive indicates Haemoglobinuria.
- Indirect fluorescent antibody test
- Complement fixation
- ELISA, dot ELISA
- In-vitro culture method
- PCR
- Latex agglutination Test.
Differential diagnosis with some of disease condition like Anaplasmosis, Thelieriosis, Leptospirosis, Trypanosomiasis, Bacillary haemoglobinuria, Post parturient haemoglobinuria, chronic copper poisoning and Rape seed poisoning etc
Treatment
- The drug of choice of babesiosis is Inj. Diminazene aceturate @ the dose rate of 3.5 mg/kg B.wt. Deep intramuscular Alternative days
- Imidocarb @the dose rate of 1.2 mg/kg B.wt. Subcutaneous route
- Long acting Inj. Oxytetracycline @the dose rate of 6.6-11mg/kg B.wt. Deep intramuscular Alternative days
- Plane Inj. oxytetracycline @the dose rate of 6.6-11mg/kg B.wt. Along with DNS intravenous route daily for 5 days
- For anemia recovery, Inj. Ferritas, Deep intramuscular Alternative days. Inj. Inferon 10ml per day and blood transfusion
- Supportive therapy like Inj. Meloxicam @the dose rate of 0.5 mg/kg B.wt. Intramuscular, Inj. Chlorphenaramine meliate @the dose rate of 0.5 mg/kg B.wt. Intramuscular, corticosteroid, fluid therapy
- Oral supplementation of Iron preparations 25-50ml per day
- In animals with Hb value below 4 mg/dl, RBC level fall below 3 Million/mm3 PCV Value below 22 are adviced for Blood transfusion of close relative donor at the rate 10-20 ml/kg B.W. to save the life of animal from anemia.
Control measures
- Elimination of tick vector :- repellent and acaricides with regular inspection of cattle may reduce the disease
- Avoid tick bites to cattle.
- In endemic area, vaccination should be done
- Cleanliness and hygienic practices in the farm.
- Regular health check up for animals.
- Quarantine for newly brought animals.
- Vaccination of healthy animals using live attenuated strains of Babesia.
References
- Review on Bovine Babesiosis and its economical importance. Journal of Veterinary Medicine and Research. Yusuf JJ(2017)
- Bovine babesiosis- OIE
- Babesiosis Fact sheet, Centre for Global Health, Division of Parasitic Diseases and Malaria.
- Diagnosis and management of bovine babesiosis outbreak in cattle in Panjab state, Mandeep singh bal, et al, Veterinary world, 2016, vol.9
- Babesiosis- Wikipedia
|
The content of the articles are accurate and true to the best of the author’s knowledge. It is not meant to substitute for diagnosis, prognosis, treatment, prescription, or formal and individualized advice from a veterinary medical professional. Animals exhibiting signs and symptoms of distress should be seen by a veterinarian immediately. |



Good one..
nice, good, informative
Good article
Nice one
Nice article
Informative article..
Nic and informative article