Common Names
Acnitis, Consumption, Great white plague, Great white scourge, Lupus vulgaris, Pearl disease, Pott’s disease, Pthisis, Rajayakshman – the king of diseases (in Hindu texts), Scrofula, Scrofuloderma, Yakshma.
Etiology
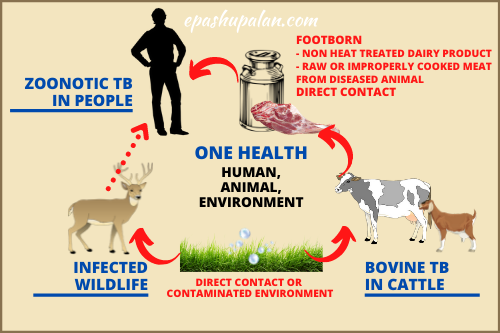
Tuberculosis is an infectious, chronic debilitating disease. Bovine tuberculosis (TB) is a chronic disease of animals caused by bacteria Mycobacterium bovis. This disease can affect practically all mammals, causing a general state of illness, coughing and eventual death. Most cases of human TB are caused Mycobacterium tuberculosis. Zoonotic TB is a form of TB in humans predominantly caused by M. bovis.
Occurrence
In developing nations, M. bovis infection is widespread. Ubiquitous, a major health related disease in developing countries like India where TB is widely prevalent among cattle, buffaloes and pigs.
Host range and reservoir
tuberculosis finds its reservoir mainly in man whereas M. bovis in infected bovines (mainly), other domestic and wild animals, and also in man. The host range of M. bovis includes man, cattle, sheep, goat, buffalo, dog, cat, horse, pig, deer, monkey, chimpanzee, bison, elephant, marsupials, mink, moles, badgers, opossum, cockatoo, ferret, fox, hare and parrot. Cases of generalized TB due to M. avium have also been reported.
Transmission
The disease is contagious and spread by contact with infected domestic and wild animals, contaminated articles or dust, including direct infection through mucous membrane or abraded skin or wound. M. bovis infected bovines (mainly) as well as other livestock kept for milk and meat production such as goats, buffaloes, sheep, camels and deer serve as source of infection not only for other domestic and wild animals but also for humans through the consumption of contaminated water, meat, milk and other dairy products. The tubercle bacilli from infected persons are effectively transmitted to the susceptible persons mainly through respiratory route. Man is also able to infect animals with both, the bovine strain (M. bovis) and the human strain of the tubercle bacilli. Direct airborne transmission of M. bovis has also been reported from infected animals or animal products to humans as well as among humans. Infection from humans to animals can occur through aerosol or by consumption of infected feed or hay by infected farm workers. However, the infection of cattle by the human strain is usually transient and self-limiting, and there are no recorded instances of cow-to-cow, or cow-to-man transmission of it.
Clinical Signs in Animals
Animals affected with TB may not show any observable symptoms.
In cattle: Swelling of superficial lymph nodes. Affected udder, will show a progressive hardening and swelling. Milk becomes thin and watery with yellow flakes in it. The generalized TB cases of years standing show emaciation (hide bound condition), cough, dry and harsh body coat, dull and sunken eyes, with occasional diarrhoea with capricious appetite, fluctuating body temperature, and at times, snoring due to involvement of retropharyngeal lymph node. In cutaneous TB, lumpy swelling, sometimes indicated by cording, occurs on the lower part of the front legs and rarely on hind legs.
In poultry: Severe emaciation, pale mucous membrane, intermittent diarrhoea are seen commonly.
Clinical Signs in Humans
Clinical tuberculosis occurs in 3 stages:
Primary tuberculosis
The lung infection results in the formation of the tubercles, center of which may break down into necrotic, caseous lesions and gradually heal by calcification.
Secondary tuberculosis
The organism drain into the bronchial tubes and upper respiratory tract. The patient shows violent coughing, greenish or bloody sputum, fever, anorexia, weight loss, extreme fatigue, night sweats and chest pain.
Extrapulmonary tuberculosis
During course of secondary tuberculosis the bacilli disseminate rapidly to other organs, as regional lymph nodes, kidneys, long bones, genital tract, brain and meninges. Urinary system is affected resulting in necrosis and scarring of renal medulla, pelvis, ureters and bladder. Reproductive organs are also affected. TB of bones and joints (vertebral column) results in paralysis and sensory loss. Tuberculous meningitis can result into mental deterioration, permanent retardation, blindness and deafness. In young ones condition known as ‘Scrofula’ occurs where settles in cervical and, less frequently, axillary lymph nodes primarily as a result of alimentary infection and dissemination, whereas, in adults post primary pulmonary disease is more common.
Besides these, Infection through skin wound causes, lesions in skin, tendon and localized lymph node lesions among persons handling infected carcasses may also occurs.
Diagnosis
In Animals
- Isolation and identification of the pathogen- It remains the only confirmatory test but requires viable bacilli, and the growth of M. bovis may take 6-8 weeks.
- Delayed type hypersensitivity– These include- (i) Single intradermal tuberculin test, (ii) Stormont test, (iii) Short thermal test, (iv) Subcutaneous tuberculin test and (v) Opthalmic test.
- Animal inoculation- The suspected material commonly milk is inoculated into the thighs of guinea pigs which results into typical lesions of tuberculosis of liver, spleen and lymph nodes of infected animals.
- PCR assays such as multiplex PCR,
- Gamma-interferon (IFN-g) assay- more sensitive than skin test but remains costly and inconvenient
- ELISA test
In Humans
- Isolation of the pathogen- It remains the only confirmatory test.
- Acid fast staining– The sputum or other specimen from the suspected cases must be tested by acid fast staining.
- Several variations in acid fast stains are available as Ziehl-Neilsen stain fluorescent stain.
- Roentgenography- Chest x-rays or roentgenographs.
- Mantoux test- 0.1 ml of PPD is injected intradermally into the forearm to see for any immediate small bleb and, the site is observed for an induration after 48 and 72 hours.
- Modern techniques– Radiometric determination of bacterial growth, Gas chromatography, DNA hybridization and
- Nucleic acid probes.
Public health implications
Mycobacterium bovis is not the major cause of human tuberculosis, which is caused by M. tuberculosis, but humans are susceptible to bovine TB. M. tuberculosis infection in humans primarily affects the lungs, although may be extra pulmonary at times. Zoonotic TB in humans besides involving lungs, can also affects extra pulmonary sites, including lymph nodes and other organs. The risk for disease increases in areas where bovine tuberculosis is endemic and where people live in conditions that favour direct contact with infected animals (ie, farmers, veterinarians, and slaughterhouse workers) or animal products (unpasteurised milk and untreated animal products).
Unique challenges
Challenges related with zoonotic tuberculosis needs to be addressed because of following facts.
- bovis is responsible for TB primarily in cattle, and also causes human disease which is indistinguishable with regard to pathogenesis, lesions and clinical findings.
- The true incidence of zoonotic tuberculosis remains unnoticed because of the absence of routine surveillance data.
- Zoonotic TB poses challenges for effective patient treatment and recovery, as bovis is naturally resistant to pyrazinamide, rifampicin and isoniazid, the common first-line anti-TB treatment drugs and also patients with zoonotic TB may receive inadequate treatment due to lack of proper diagnosis. This may lead to development of multidrug-resistant TB (MDR-TB) to other anti-TB drugs, which poses a major threat to human health globally.
Prevention and Control
- Regular health checkup for occupational groups at risk.
- Proper abattoir controls with dissemination of information to the butchers and farmers regarding bovis
- Promotion of milk pasteurization and increased awareness about avoiding consumption of raw, inadequately cooked and contaminated meat or unpasteurized milk and other dairy products.
- Education and training of health workers.
- BCG vaccination and preventive chemotherapy.
- Wearing of protective clothing and personal hygiene.
- Develop capacity of the animal health sector to reduce the prevalence of TB in livestock.
- Try to address constraints of humidity, poor ventilation, overcrowding, poor nutrition, improper housing, unhygienic conditions faced by animals.
- Handling of carcasses, infected tissue with caution and burial of carcasses of infected animals deep in to ground.
- Increase awareness of zoonotic TB and establish effective intersectoral collaboration.
- Implementation of elimination programme with particular attention to diagnosis, movement and trading of animals
- Develop and implement policies and guidelines for the prevention, surveillance, diagnosis, and treatment of zoonotic TB, in line with intergovernmental standards where relevant.
References
- Roadmap for Zoonotic Tuberculosis. WHO, OIE, FAO and The Union, 2017.
- FAO – Animal Production and Health: http://www.fao.org/ag/againfo/home/en/index.htm.
- OIE: http://www.oie.int/
- The Union – Zoonotic TB subsection: http://www.theunion.org/news-centre/features/member-highlight-the-zoonotic-tb-sub-section.
- WHO – The End TB Strategy: http://www.who.int/tb/strategy/en/
- https://www.cdc.gov/features/tbsymptoms.
- Michel AL, Geoghegan C, Hlokwe T, Raseleka K, Getz WM, Marcotty T. Longevity of Mycobacterium bovis in raw and traditional souring milk as a function of storage temperature and dose. PLoS One 2015; 10:
- Cosivi O, Grange JM, Daborn CJ, et al. Zoonotic tuberculosis due to Mycobacterium bovis in developing countries. Emerg Infect Dis 1998; 4: 59–70.
| The content of the articles are accurate and true to the best of the author’s knowledge. It is not meant to substitute for diagnosis, prognosis, treatment, prescription, or formal and individualized advice from a veterinary medical professional. Animals exhibiting signs and symptoms of distress should be seen by a veterinarian immediately. |






1 Trackback / Pingback