Lumpy skin disease is a vector borne, neglected viral disease caused by lumpy skin disease virus, a member of Capripoxvirus genus of Poxviridae family. It is an infectious, contagious and transboundary disease of economic importance affecting cattle and buffaloes. It causes eruptive skin lesions, occasionally fatal disease of cattle characterized by nodular growth on the skin and other parts of the body. Generally, fever, anorexia, and characteristic nodules on the skin mucous membrane of mouth, nostrils, udder, genital, rectum, drop in milk production, abortion, infertility and sometimes death are the clinical manifestations of the disease. The condition of the affected animals aggravates further by the involvement of secondary bacterial infections. Lumpy skin disease is commonly found in southern and eastern Africa, but in the 1970s it extended northwest through the continent into sub-Saharan West Africa. Since 2000, it has spread to several countries in the Middle East countries including India.
Species affected
It is mainly a disease of cattle but the range of animal species that may be infected and develop clinical disease is uncertain but it is probably wider than cattle and Asian water buffaloes (Bubalus bubalis); there are conflicting reports concerning the buffaloes (El-Nahas et al. 2011, OIE 2002, Coetzer et al. 2018).
All ages of cattle and both sexes are susceptible to infection (Weiss 1968) although on occasion cows have been only mildly affected while their calves developed more typical and severe lesions 24 to 48 hours earlier than their dams (Le Roux 1945). More severe disease has been reported in breeds of exotic cattle i.e. Holstein Friesian, especially those with thin skins such as Friesians and in other high-producing European dairy breeds. Cows in peak lactation seem also to be more severely affected (Coetzer et al. 2018). It has been observed that Holstein Friesian cattle or crossbred cattle are more susceptible to LSD as compared to zebu cattle (OIE 2002).
Etiology
Lumpy skin disease (LSD) caused by lumpy skin disease virus (LSDV) which is related to that of sheep pox. LSDV is a member of the genus Capripoxvirus within the subfamily Chordopoxvirinae, family Poxviridae. The prototype strain is known as the Neethling poxvirus (OIE 2002, Coetzer et al. 2018).
Though LSDV virus is susceptible to 55°C for 2 hours, 65°C for 30 minutes, however, it is highly stable and is recoverable for at least 18 days from air-dried hides kept at room temperature, 10 years from skin nodules kept at –80°C and from infected tissue culture fluid stored at 4°C for six months (Weiss 1968, OIE 2002). The virus was reported to persist in necrotic skin nodules for up to 33 days or more, desiccated crusts for up to 35 days, and at least 18 days in air-dried hides (OIE 2002).
The LSDV is susceptible to alkaline or acid pH however, between pH 6.6 and 8.6 virus preparations showed no significant reduction in titre after exposure to a temperature of 37°C for five days (OIE 2002). Therefore, the hide of succumbed animals may contribute in the propagation and transmission of the virus.
The LSDV virus is susceptible to ether (20%), chloroform, formalin (1%), and some detergents, e.g. sodium dodecyl sulphate. It is also susceptible to phenol (2% for 15 minutes), sodium hypochlorite (2–3%), iodine compounds (1:33 dilution), Virkon® (2%), quarternary ammonium compounds (0.5%) (OIE 2002).
It can remain viable for long periods in the environment. The virus is susceptible to sunlight and detergents containing lipid solvents, but in dark environmental conditions, such as contaminated animal sheds, it can persist for many months (OIE 2002).
History
Lumpy skin disease appears epidemically or sporadically. Frequently, new foci of infection appear in areas far removed from the initial outbreak. It’s incidence is highest in wet summer weather, but it may occur in winter. It is most prevalent along water courses and on low ground. The LSD is endemic in African and Middle East countries but has started spreading to Asian and other countries. It has been recently reported from China and Bangladesh sharing borders with India. In August 2019, LSD has been reported first time in Odisha State of India with 7.1% morbidity among cattle (Sudhakar et al. 2020).
The first outbreak of LSD was reported from Zambia 1929 (Alexander et al. 1957) and the disease was called as pseudo-urticaria (Weiss 1968).
In 1943, the condition was considered to be due to photosensitization (Quin and Dori 1943) but the actual cause of the disease i.e. LSDV was isolated in 1943 as capripoxvirus (Alexander et al. 1957) and the was first recognized as an infectious condition in 1943 following an outbreak in Ngamiland, Northern Botswana (Von Backstrom 1945).
Towards the end of 1944 LSD was reported from South Africa where it spread rapidly throughout the country despite enforcement of control measures and the disease was coined as ‘Knopvelsiekte’ though also described as Pseudo Urticaria or Lumpy Disease, Ngamiland Cattle Disease (Thomas and Mari 1945).
In 1947 the disease had become enzootic in South Africa and had also been reported from Swaziland, Basutoland and Portuguese East Africa and subsequently from Madagascar, Tanganyika and the Belgian Congo (Diesel 1949, Haig 1957).
In 1956, it was reported from Central and East Africa and in 1957 LSD outbreak was reported in Kenya (MacOwan 1959); since then it has occurred widely in Africa and in Madagascar (Coetzer et al. 2018).
In 1983 LSD was reported from Ethiopia and in 1988 from Egypt, Israel in 1989, Bahrain and Reunion in 1993, although those outbreaks were not confirmed by virus isolation (Coetzer et al. 2018)
In 2006 and 2007 LSD was reported again in Egypt (Salib and Osman 2011) and Israel and in 2009 occurred in Oman (Brenner et al. 2009).
In 2012 – 2013, LSD reappeared in northern Israel (Ben-Gera et al. 2015) and then spread swiftly in the Middle East, being reported in Lebanon, the Palestinian Autonomous Territories and Jordan and caused huge economic losses (Abutarbush et al. 2015).
In 2013, outbreaks of LSD were also reported Turkey (Timurkan et al. 2016), Kuwait, Saudi Arabia and Iraq (Al‐Salihi and Hassan 2015).
In 2014, outbreaks of LSD were reported in Iran (Sameea et al. 2017) and the northern part of Cyprus as well as in Saudi Arabia and Bahrain. It then spread northeast through the Caucasus, affecting Azerbaijan (Tasioudi et al. 2016).
In 2015, it was reported from Armenia and the Russian Federation. Lumpy skin disease was reported for the first time in the European Union from Greece in 2015; it probably originated in Thrace (Turkey). The disease emerged again in Greece from April to November 2016 (Coetzer et al. 2018).
In 2016, LSD occurred in Georgia and Kazakhstan. In 2016 LSD spread to Bulgaria, Serbia, Montenegro, Kosovo and Albania. In the same year it was reported again in Iran and Iraq as well as Azerbaijan (Coetzer et al. 2018).
Information is also provided by Food and Agriculture Organization on the incursion risk of LSD to Central Asia and Europe and distribution maps of outbreaks occurred between 2013-2017 in the Middle East, Turkey, the Balkans and Eastern Europe/ Central Asia (FAO 2017).
In August 2019, LSD has been reported first time in Odisha State of India (Sudhakar et al. 2020) and now in 2020, the disease is prevalent in Maharashtra and Madhya Pradesh. It may be alarm for Pan India.
Transmission
The transmission of LSDV is not clear but it has been reported that the disease is transmitted by arthropod vectors (Gupta et al. 2020). Experimentally, three species of hard ticks found in Africa have been shown to biologically transmit the virus. As the disease can be experimentally transmitted by infected saliva, contact infection is considered as another route of infection. African buffalo are suspected as maintenance hosts in Kenya (MVM 2020).
- Vectors: Aedes aegypti female mosquitoes and sheep head flies are capable of the
mechanical transmission of LSDV from infected to susceptible cattle (Chihota et al. 2001, Kitching & Mellor 1986). Mosquitoes fed upon lesions of cattle infected with LSDV were able to transmit virus to susceptible cattle over a period of 2–6 days post-infective feeding. (Wallace et al. 2006). An abundance of the Stomoxys flies (Figure 1.) was associated with outbreaks of LSD. The transmission studies reveal that Rhipicephalus (Boophilus) appendiculatus (brown ear tick – Figure 2) males transmit LSDV mechanically. Similarly, decoloratus, females were shown to transmit the virus via their eggs to larvae, which in turn, were able to infect the cattle (Coetzer et al. 2018).

- Semen: The LSDV has been isolated from the semen of inapparent diseased bulls (Weiss 1968, Irons et al. 2005, Sudhakar et al. 2020). Transmission of LSDV via artificial insemination has also been shown experimentally (Annandale et al. 2014).
- Fomites: Transmission did occur when common drinking and feeding troughs were used, thus confirming the suspicion that infected saliva may contribute to the spread of the disease (Coetzer et al. 2018).
- Direct contact: The disease is transmissible to suckling calves through infected milk and infected cows have been reported to give birth to calves with skin lesions (Coetzer et al. 2018).
- Iatrogenic transmission via contaminated needles during vaccination or other injections may also occur (Coetzer et al. 2018).
- The outbreaks depend on animal movements, immune status, wind and rainfall patterns affecting vector populations.
Socio-economic impact
The LSDV usually causes 10 – 20% morbidity and 1 – 5% mortality among the livestock (OIE2017), but other studies have reported 100% morbidity (Gupta et al. 2020). Usually, mortality rate is 1 – 5% (OIE 2002), however, it is variable depending on the strain of virus and its virulence and susceptibility of host; 50% in young animals, 5% in adults (FAO 1994).
LSD is economically important because of its prolonged debilitating effects in severely afflicted animals including reduced weight-gain, temporary or permanent cessation of milk production, sometimes accompanied by mastitis, temporary or permanent infertility or even sterility in bulls as a consequence of orchitis, as well as permanent skin damage. Abortion may follow infection in approximately 10% of pregnant cows (Coetzer et al. 2018).
Public Health Concern
LSDV is not a zoonotic disease (OIE 2002) but it causes huge production losses to the farmers.
Incubation period
The incubation period is ranged from 8–15 days until the onset of fever (Coetzer & Tuppurainen 2004).
Clinical Signs
The Lumpy Skin Disease is range from acute and severe to subclinical and is characterized by pyrexia, lymphadenopathy and skin nodules. The lesions can affect internal organs such as the stomach (Wallace & Viljoen 2005).
The affected animals have fluctuating body temperature (105.8°F), diarrhoea, nasal discharge and salivation. The pregnant animals may abort and become infertile. The first lesion appears in perineum (FAO 1994).
Typically, the affected cattle develop a febrile response one to two weeks after exposure to the virus. Animals remain febrile for four to 14 days, during which time excessive salivation (Figure 3), lachrymation and a mucoid nasal discharge are evident. The nasal discharge later becomes mucopurulent. Lachrymation may be followed by conjunctivitis, and in a few cases erosions are present in the mucosae of the conjunctivae, ultimately resulting in corneal opacity and blindness (Figure 4). In the majority of affected cattle the superficial lymph nodes are enlarged.

Skin nodules, the characteristic feature of the disease, usually appear two to five days after the initial febrile response (Figure 5, 6). The nodules, which are randomly distributed and range in diameter from 10 to 30 mm, involve both the skin and subcutaneous tissues and sometimes even the underlying musculature. The size of the nodules is usually fairly uniform but several nodules may fuse to form large, irregularly circumscribed nodules or plaques. The number of nodules may range from a few to several thousand in severely affected animals. The nodules are well-circumscribed, firm, round and raised (Figure 7) and are particularly conspicuous in short-haired animals. In long-haired cattle the nodules are often only recognized when the skin is palpated or moistened. In most cases, nodules are particularly noticeable on the perineum and the vulva. On cross-section, the skin nodules in acute or subacute stages of infection are reddish-grey and the dermis and subcutaneous tissues oedematous.104 The subcutis is often infiltrated with a reddish-grey serous fluid. Skin lesions either resolve, become indurated (in which case they persist as hard lumps or ‘sitfasts’ for 12 months or longer) (Figure 7) or sequestrate to leave deep ulcers (Figure 8), partly filled with granulation tissue that often suppurates.

In severe acute cases, the ventral parts of the body, i.e. dewlap, brisket, ventral abdomin, thorax and the legs (Figure 9) may be slightly too severely oedematous one to two days before the appearance of the nodules and remain so for a week or more. Nodular skin lesions may extend into underlying tissue such as tendons and tendon sheaths resulting in lameness in one or more legs (Figure 10).

Most affected animals have multifocal, roughly circular, necrotic areas 10-20 mm in diameter on the muzzle (Figure 11) and and buccal cavity, the inside of the lips, gingivae, dental pad (Figure 12) and upper palate (Figure 13).

The lesions may also be present in the udder, and teats (Figure 14), vagina ((Figure 15) and the testes got atrophied following orchitis (Figure 16).

Post mortem lesions
In the respiratory tract (nasal cavity, larynx, trachea and bronchi) and buccal cavity (the inside of the lips, gingivae and dental pad); these lesions may also be present in the fore-stomachs, abomasum, uterus.
In the upper respiratory tract i.e. nasal turbinate (Fugure 17) larynx and pharynx greyish-yellow foci of necrosis (Figure 18) may seen clearly and in larynx and trachea (Figure 19) multiple, well-circumscribed, necrotic areas of about 10-20 mm in diameter are common in severe clinical cases. These necrotic tissues may dislodge and be inhaled, resulting in pneumonia. Stenosis of the trachea may follow healing of these lesions (Figure 20) with scar tissue formation some weeks or months after the acute stage of the disease.
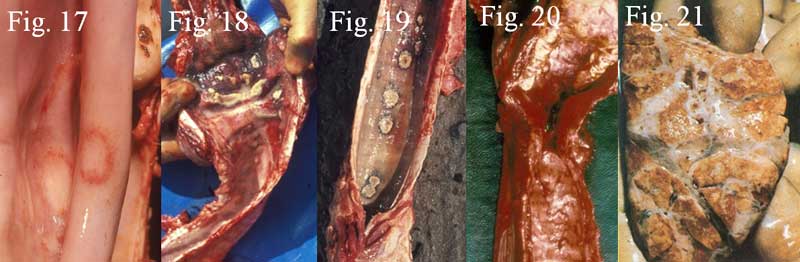
The other post mortem lesions observed in LSD are ulcerative lesions in the mucosa of the respiratory and digestive tract; reddish, haemorrhagic to whitish lesions in the lungs; oedema (interlobular) and nodules in the lungs (Figure 21); heart lesion (endocardium); thrombosis of skin vessels followed by cutaneous infarction and sloughing (FAO 1994).
Differential diagnosis
Allergies, screw-worm myiasis, urticaria, dermatophilosis (streptothricosis), bovine herpes dermophatic infection, cattle grubs, vesicular disease, bovine ephemeral fever, photosensitization, besnoitiosis (elephant skin disease), sweating weakness of calves, bovine farcy and skin form of sporadic bovine lymphomatosis (FAO 1994).
Treatment and Control
There is no specific antiviral treatment available for LSD affected cattle. Sick animals may be removed from the herd and given supportive treatment consisting of local wound dressing to discourage fly worry and prevent secondary infections. In most instances mildly affected animals with only a few skin nodules will recover without any treatment while those that are severely affected should be provided with quality palatable feed and should be well cared for (Coetzer et al. 2018). Systemic antibiotics may be given for skin infections, cellulitis or pneumonia, and food and water should be made readily available (Davies 1991).
- It has been observed that vector control along quarantine could be helpful but no apparent benefits have been observed (Davies 1991). However, vaccination along with strict quarantine measures and vector control could be effective for preventing the spread of the disease (Coetzer et al. 2018).
- Control and eradication of LSD in epidemic areas, relies on early detection of the cases, followed by a rapid and widespread vaccination campaign, in combination with stopping of cattle movement control (Coetzer et al. 2018).
- Import restrictions on domestic cattle and water buffaloes, and selected products from endemic areas or countries.
- Surveillance measures to detect LSD are recommended over a distance of at least 20 kilometres from an infected country or zone (OIE 2002).
- Proper disposal of dead animals (e.g. incineration), and cleaning and disinfection of premises and implements are recommended for LSD.
EVP formulation for Lumpy Skin Disease For oral administrations
- Blend 10 betel leaves, 10 g black pepper and 10 g salt to form a paste. Now, mix it with jaggery. Feed this one dose every three hourly for first day and afterwards thrice a day for next 2 weeks (Punniamurthy).
- Blend garlic – 2 pearls, Coriander – 10 g, Cumin – 10 g, Tulsi – 1 handful, Dry cinnamon leaves – 10 g, Black pepper – 10 g, Betel leaves – 5 nos, Shallots – 2 bulbs, Turmeric powder – 10 g, Chirata leaf powder – 30 g, Sweet basil – 1 handful, Neem leaves – 1 handful, Aegle marmalos (Bel) leaves – 1 handful and Jaggery – 100 g, to make paste. Now, mix it with jaggery. Feed this one dose every three hourly for first day and afterwards twice a day till the condition resolves (Punniamurthy).
- If there are wounds on skin, blend acalypha indica leaves -1 handful, Garlic – 10 pearls, Neem leaves – 1 handful, Turmeric powder – 20 g, Mehndi leaves – 1 handful, Tulsi leaves – 1 handful to make a paste. Now, mix it with 500 ml coconut or Sesame oil and boil and bring it to cool. Before applying the paste thoroughly clean the wounds and then apply directly over the affected skin (Punniamurthy).
- If maggots are seen in the wounds, then apply Anona leaf paste or camphorated coconut oil for the first day only if maggots are present.
References
- Abutarbush, S.M., Ababneh, M.M., Al Zoubi, I.G., Al Sheyab, O.M., Al Zoubi, M.G., Alekish, M.O. and Al Gharabat, R.J., 2015. Lumpy Skin Disease in J ordan: Disease Emergence, Clinical Signs, Complications and Preliminary‐associated Economic Losses. Transboundary and emerging diseases, 62(5), pp.549-554.
- Alexander, R.A., Plowright, W. and Haig, D.A., 1957. Cytopathogenic agents associated with lumpy skin disease of cattle. Bulletin of epizootic diseases of Africa, 5, pp.489-492.
- Al‐Salihi, K.A. and Hassan, I.Q., 2015. Lumpy skin disease in Iraq: study of the disease emergence. Transboundary and emerging diseases, 62(5), pp.457-462.
- Annandale, C.H., Holm, D.E., Ebersohn, K. and Venter, E.H., 2014. Seminal transmission of lumpy skin disease virus in heifers. Transboundary and emerging diseases, 61(5), pp.443-448.
- Ben-Gera, J., Klement, E., Khinich, E., Stram, Y. and Shpigel, N.Y., 2015. Comparison of the efficacy of Neethling lumpy skin disease virus and x10RM65 sheep-pox live attenuated vaccines for the prevention of lumpy skin disease–The results of a randomized controlled field study. Vaccine, 33(38), pp.4837-4842.
- Brenner, J., Bellaiche, M., Gross, E., Elad, D., Oved, Z., Haimovitz, M., Wasserman, A., Friedgut, O., Stram, Y., Bumbarov, V. and Yadin, H., 2009. Appearance of skin lesions in cattle populations vaccinated against lumpy skin disease: statutory challenge. Vaccine, 27(10), pp.1500-1503.
- Chihota, C.M., Rennie, L.F., Kitching, R.P. and Mellor, P.S., 2001. Mechanical transmission of lumpy skin disease virus by Aedes aegypti (Diptera: Culicidae). Epidemiology & Infection, 126(2), pp.317-321.
- Coetzer, J.A.W, Tuppurainen, E., Babiuk, S. and Wallace, D. 2018. Lumpy Skin Disease. In book: Infectious Diseases of Livestock, Part IIPublisher: Anipedia.
- Coetzer, J.A.W. and Tuppurainen, E., 2004. Lumpy skin disease. Infectious diseases of livestock, 2, pp.1268-1276.
- Davies, F.G., 1991. Lumpy skin disease of cattle: a growing problem in Africa and the Near East. World Animal Review, 68(3), pp.37-42.
- Diesel, A.M., 1949. The epizootology of “lumpy skin disease” in South Africa. Proc. 14th International Veterinary Congress, London 2, 492–500.
- El-Nahas, E.M., El-Habbaa, A., El-Bagoury, G. and Radwan, M.E., 2011. Isolation and identification of lumpy skin disease virus from naturally infected buffaloes at Kaluobia, Egypt. Global Veterinaria, 7(3), pp.234-237.
- FAO, 1994, Manual on meat inspection for developing countries. Food and Agriculture Organization of the United Nations Rome.
- 2017. Sustainable prevention, control and elimination of Lumpy Skin Disease – Eastern Europe and the Balkans. FAO Animal Production and Health Position Paper. No. 2. Rome, Italy.
- Gupta, T., Patial, V., Bali, D., Angaria, S., Sharma, M. and Chahota, R., 2020. A review: Lumpy skin disease and its emergence in India. Veterinary Research Communications, pp.1-8.
- Haig, D.A., 1957. Lumpy skin disease. Bull. Epizoot. Dis. Afr, 5(9): 421–430.
- Irons, P.C., Tuppurainen, E.S.M. and Venter, E.H., 2005. Excretion of lumpy skin disease virus in bull semen. Theriogenology, 63(5), pp.1290-1297.
- Kitching, R.P. and Mellor, P.S., 1986. Insect transmission of capripoxvirus. Research in veterinary science, 40(2), pp.255-258.
- Le Roux, P.L., 1945. Notes on the probable cause, prevention and treatments of pseudo-urticaria and associated septic conditions in cattle. Northern Rhodesia Department of Animal Health, Newsletter, pp.1-4.
- MacOwan, K.D.S., 1959. Observations on the epizootiology of lumpy skin disease during the first year of its occurrence in Kenya. Bull. Epizootic Dis. of Africa, 7, pp.7-20.
- MVM, 2020. Lumpy Skin Disease. MSD Veterinary Manual.
- OIE, 2002, LUMPY SKIN DISEASE – Aetiology Epidemiology Diagnosis Prevention and Control References. P. 5.
- Punniamurthy N., Ethnoveterinary formulation for Lumpy Skin Disease For oral administrations. National dairy Development Board.
- Quin, J.L. and Dori J.L., 1943. A skin condition in cattle probably associated with photosensitisation. Journal of the South African Veterinary Association, 14(1), pp.10-11.
- Salib, F.A. and Osman, A.H., 2011. Incidence of lumpy skin disease among Egyptian cattle in Giza Governorate, Egypt. Veterinary world, 4(4).
- Sameea Yousefi, P., Mardani, K., Dalir‐Naghadeh, B. and Jalilzadeh‐Amin, G., 2017. Epidemiological study of lumpy skin disease outbreaks in North‐western Iran. Transboundary and emerging diseases, 64(6), pp.1782-1789.
- Sudhakar, S.B., Mishra, N., Kalaiyarasu, S., Jhade, S.K., Hemadri, D., Sood, R., Bal, G.C., Nayak, M.K., Pradhan, S.K. and Singh, V.P., 2020. Lumpy skin disease (LSD) outbreaks in cattle in Odisha state, India in August 2019: Epidemiological features and molecular studies. Transboundary and Emerging Diseases.
- Tasioudi, K.E., Antoniou, S.E., Iliadou, P., Sachpatzidis, A., Plevraki, E., Agianniotaki, E.I., Fouki, C., Mangana‐Vougiouka, O., Chondrokouki, E. and Dile, C., 2016. Emergence of lumpy skin disease in Greece, 2015. Transboundary and Emerging Diseases, 63(3), pp.260-265.
- Thomas, A.D. and Mari C.V.E., 1945. Knopvelsiekte. Journal of the South African Veterinary Association, 16(1), pp.36-43.
- Timurkan, M.Ö., Özkaraca, M., Aydın, H. and Sağlam, Y.S., 2016. The detection and molecular characterization of lumpy skin disease virus, northeast Turkey. International Journal of Veterinary Science, 5(1), pp.44-47.
- Von Backstrom, U., 1945. Ngamiland cattle disease: preliminary report on a new disease, the etiological agent being probably of an infectious nature. Journal of the South African Veterinary Association, 16(1), pp.29-35.
- Wallace, D.B., Ellis, C.E., Espach, A., Smith, S.J., Greyling, R.R. and Viljoen, G.J., 2006. Protective immune responses induced by different recombinant vaccine regimes to Rift Valley fever. Vaccine, 24(49-50), pp.7181-7189.
- Weiss, K.E., 1968. Lumpy skin disease virus. In Cytomegaloviruses. Rinderpest Virus. Lumpy Skin Disease Virus (pp. 111-131). Springer, Berlin, Heidelberg.
|
The content of the articles are accurate and true to the best of the author’s knowledge. It is not meant to substitute for diagnosis, prognosis, treatment, prescription, or formal and individualized advice from a veterinary medical professional. Animals exhibiting signs and symptoms of distress should be seen by a veterinarian immediately. |







2 Trackbacks / Pingbacks