Toxicology : It is the study of nature and effects of poisonous or toxic substances.
Toxicity : It is inherent capacity of substance to produce harmful effects.
Poison : It is any substance (liquid/solid/gas) that causes deleterious effects in a living organism.
Venoms : These are substances produced by reptiles for their defense mechanism. E.g. Snake Venom.
Toxins : These are the poisonous substances produced in animal tissues by the action of bacteria or waste products that are not recovered from body due to liver or kidney failure.
Antidote : These are the drugs or chemical agents that neutralize the effects of poison.
SOURCES OF POISONING
There are two major sources of poisoning in animals –
- Natural Sources.
- Human oriented sources.
1. Natural Sources
- Plants : Ipomea carnea, Datura alba, Atropa belladonna, Strychnus nuxvomica, Young shoots of sorghum, Nitrate rich plants.
- Animals : Poisonous snake bite (Cobra, Krait, Russel viper and Rattle snake). Scorpion bite, Toad toxin, Tick toxins and Spider venom.
- Minerals or metals : Arsenic, Lead, Mercury, Selenium, Fluoride.
2. Human oriented sources
2.1 Accidental causes
- Fertilizers : Urea, phosphate or Nitrate fertilizers.
- Insecticides : Organophosphates, Organochlorines, Carbamates, Pyrethroids.
- Rodenticides : Zinc phosphide.
- Industrial effluents : Lead, Fluorine, Cyanide, Mercury, Nitrate.
- Radiation hazards.
2.2 Malacious poisoning
Unlawful discriminal killing of animals by administering poisons E.g. Zinc phosphide, Strychnine, Abrus etc.
CLASSIFICATION OF POISONING
The classification of poison on the basis of its effecr on body is as follows:
1. Poisons causing respiratory insufficiency (anoxia) by
- Hindering oxygen uptake from pulmonary alveoli
E.g. Petroleum products, Nitrous oxide, Sulfur oxide. - Hindering oxygen transport to tissues
E.g. Nitrites/Nitrates – Formation of Methaemoglobin. - Inhibiting oxygen utilization by tissue cells
E.g. HCN/Cyanide – Inhibiting enzyme cytochrome oxidase.
2. Poisons causing nerbous stimulation or depression by
- Directly damaging the brain or spinal cord
E.g. Salt, Organomercurials. - Acting on known receptor sites
E.g. Organophosphates and Carbamate pesticides – inhibits enzyme acetyl cholinesterase. - Causing nervous stimulation or depression by unknown mechanism
E.g. Chlorinated hydrocarbons, Lead, Acute Fluoride poisoning.
3. Poisons causing severe liver damage
E.g. Aflaxtoxins and other mold toxins.
4. Poisons causing severe kidney damage
E.g. Mold toxins, Carbamates.
5. Poisons causing severe colic
- Direct corrosives/irritants E.g. Chemicals.
- Metabolic poisons E.g. Arsenic, Urea.
6. Poisons causing bone, tooth, hoof and hair abnormalities
E.g. Fluorosis, Selenium toxicosis.
7. Poisons causing lesions on skin
E.g. Corrosives (acid/alkalies), Mold toxins, Photosensitizing plants like Lantana Camara, Tribulus species.
TYPES OF TOXICITY
- Acute Toxicity : It results from exposure of animals to high dose of a compound usually a single exposure or exposure over a short period. The animals exhibit immediate onset of severe toxic symptoms and usually die suddenly.
- Subacute toxicity : Slow development of toxicity on repeated exposure to sub toxic doses of a compound over a period up to 90 days.
- Chronic toxicity : It results from exposure to still less doses than in subacute toxicity over a period of 6 months or more.
MECHANISM OF ACTION
The mechanism by which poisons of various kind produce their toxicity is mentioned as below:
- Local injury to tissue – acids, alkalis, heavy metals, venom – snake, bee stings.
- Necrosis of epithelial cells – certain plant toxins, thallium, cresols or phenols.
- Functional effect of CNS without lesions – strychnine, chlorinated hydrocarbons, hydrocyanic acid.
- Injury to blood and vascular system – hemolysis (lead, copper, castor bean, nightshades, phenothiazine, saponins), bone marrow (benzene, trichloroethylene, brackenfern, crotalaria, radioactive compounds, high intake of vitamin A), injury to endothelium (ergot, thallium), methaemoglobin (nitrous oxide, chlorates), clotting malfunction (warfarin, dicoumarol).
- Blocking enzyme systems – arsenic (Sulfhydryl, Phosphate tie-up), organophosphates (cholinesterase), hydrocyanic acid (cytochrome oxidase), sodiumfluoroacetate (TCA cycle), heavy metals in general.
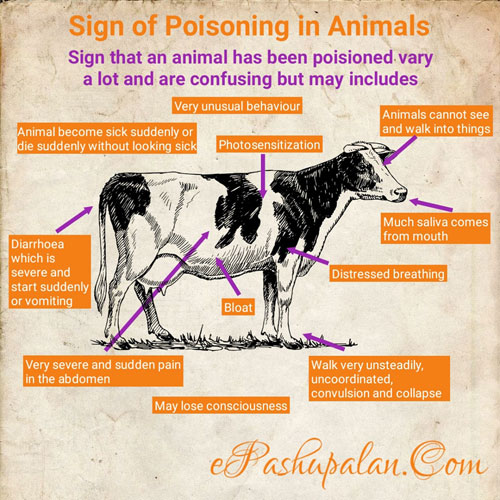
DIAGNOSIS OF POISONING CASES
1. Types of evidence
- History or circumstantial
- Symptomatic
- Pathologic
- Chemical
- Experimental
2. Obtaining the history – Most Important.
3. Did animals have access to the toxicity?
4. Was there sufficient amount of material to cause clinical signs or death?
5. In the case of plants, is there evidence that the toxic plants were eaten?
GENERAL PRINCIPLES OF TREATMENT OF POISONING
Depending upon tentative, presumptive or confirmative diagnosis and health status of poisoned animal treatment is given. The treatment is broadly divided into five categories.
1. General Procedures
- Removal of source of poison : shifting animal to fresh feed and water.
- Removal of unabsorbed toxicant from GI tract and skin
a) If poison is ingested then it can be removed by using-
- Gastric lavage with neutralizing agent or water.
- Emetics : g. 30-60 gm of common salt in a glassful warm water.
- Purgatives: g. Saline purgatives are beneficial for removal of non-irritant poisons. e.g. Magnesium Sulphate @ 250-500 gm orally in large animals.
- Oily purgatives are preferred in case of irritant poisons.
b) If the source of poisoning is through eye or skin then –
- Wash the skin thoroughly with lot of water (Avoid scrubbing)
- Wash the eyes with water or normal saline.
2. Removal of absorbed toxin– Intensive fluid therapy (Inj. Dextrose 5%) to promote excretion of toxin.
3. Common Antidotal Therapy
This comprises administration of neutralizing or detoxifying agents.
- Use of universal antidote (2 parts activated charcoal + 1 part Tannic acid + 1 part Magnesium oxide). Dose : 250 gm for large animals, 15-30 gm for small animals.
- Administration of egg white (from 6-8 eggs) and milk (500 ml) orally to neutralize heavy metals.
- Use of 15-20 drops of tr. Iodine in 100-125 ml of drinking water to precipitate alkaloids, strychnine, mercury and lead.
- Use of 5% acetic acid or vinegar or lemon juice to dilute alkali poisons.
- Use of lime water, powdered chalk to dilute acid poisons.
4. Specific antidotal Therapy
It is the use of exact antidote against certain poisoning on its confirmation.
| Poisoning | Specific Antidote |
| Mercury | BAL (Dimercaprol) |
| HCN poisoning | Sodium nitrite and sdium thiosulphate. |
| Nitrate poisoning | Methylene blue |
| Organophosphate poisoning | Atropine sulphate |
| Lead poisoning | Ca disodium EDTA |
| Arsenic | BAL (Dimercaprol), d-penicillamine, Sodium thiosulfate |
| Iron | Defroxamine |
| Zinc | Calcium disodium EDTA |
| Cyanide | Sodium nitrite, Sodium thiosulfate |
| Opiates | Nalorphine |
| Alkaloids | Tannic acids |
| Fluorides, oxalates | Calcium Gluconate |
| Barbiturates | Bemegride |
| Copper | Penicillamine molybdenum salts, Ammonium molybdate, Sodium sulfate |
| Molybdenum | Copper Sulphate |
| Organophosphate compounds | Cholinesterase reactivators (oximes) |
| Coumarin anticoagulants | Vitamin K1 |
| Ethylene glycol, methyl alcohol | Ethanol |
| HCN poisoning | Sodium nitrite and sodium thiosulphate. |
| Nitrate poisoning | Methylene blue |
| Organophosphate poisoning | Atropine sulphate |
| Lead poisoning | Ca disodium EDTA |
| Plant Toxicities | Antidotes |
| Cyanogenic Plants | Sodium nitrate, Sodium thiosulfate |
| Oxalates | Lime water |
| Nitrate and Nitrite Toxicity | Methylene blue |
| Abrus Poisoning | Antiabrin serum |
| Kaner | Atropine Sulfate, antihistamine |
| Caster | Ricin antiserum |
| Sweet clover poisoning | Vitamin K |
| Bracken fern poisoning | Butyl alcohol, Thiamine hydrochloride |
| Selenium Poisoning | Magnesium sulphate |
| ANTU poisoning | No specific Rx |
| Warferin poisoning | Diazepam/Vitamin K |
| Aflatoxicosis | Activated charcoal |
| Insecticides poisoning | Antidotes |
| Organophosphorus compounds | Atropine sulfate, Monoxime |
| Organochlorine compounds | Activated charcoal |
| Snake bite | Mono or polyvalent antivenim therapy |
| Bromide | Chloride |
| Urea | Vinegar or 5% acetic acid |
| Mimosine | Steam processing or FeSO4 salt |
| Bee stings | Sodium bicarbonate |
| Cottonseed cake | 1% Calcium hydroxide or 1% FeSO4 |
| Linseed meal | Cake can be detoxicated by soaking in water and then boiling for 10 minutes to eliminate the hydrocyanic acid. |
| Soyabean meal | Butyl alcohol, Thiamine hydrochloride |
| Coal tar/phenol/cresol/Lysol poisoning | Magnesium or sodium sulphate |
| Strychnine poisoning/Nuxvomica | Tannic acids |
5) Symptomatic Treatment
It comprises the treatment based on symptoms
- Maintenance of clear air way.
- Use of respiratory stimulants.
inj Nikethamide @ 7-11 mg/kg IM,IV. - Control of convulsions by using sedatives.
inj Diazepam @0.5-1 mg/kg IM, IV. - Giving CNS stimulants in case of severe depression.
E.g. Caffeine 0.5 g IV (Dog 0.1-1.0 g SC) - In case of shock, protection of the animal from cold and use of corticosteroids / adrenaline and fluid therapy.
- Intensive fluid therapy to counteract dehydration owing to diarrhea or vomition.
- Oral administration of demulcents (mixture of egg, sugar and milk or rice gruel) to alleviate irritation caused by poisons.
6) Supportive Treatment
This is given during and after recovery from poisoning.
- Liver tonics to promote appetite and liver function.
- Fluids and electrolytes to compensate water and electrolyte losses.
- Dextrose to compensate lost energy.
- Antibiotics to check secondary bacterial infections.
References
- U. Bhikane and S.B. Kawitkar (2016). Handbook for Veterinary Clinicians., Krishana Pustakalaya, 254-259 pp.
- K. Roy (2009). A Textbook of Veterinary Pharmacology and Toxicology., Kalyani Publishers, 1-605pp.
- Satish Kumar Garg (2000). A Textbook of Veterinary Toxicology., CBS Publishers and Distributors Ltd. 1-321 pp.






Thoroughly explained