Abstract
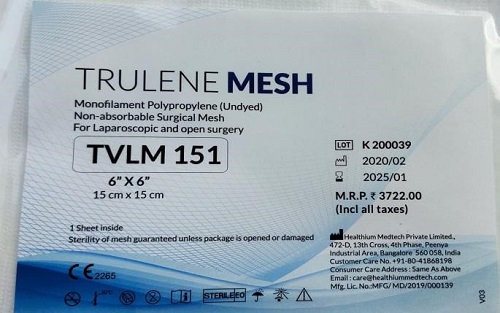
In this case study polypropylene mesh was used to facilitate reconstruction of large tissue defects by tension-free repair in a female crossbreed calf with hernial ring size around 9 cm. Umbilical hernia is the the most common form of congenital hernia in calves..The calf was operated by keeping polypropylene mesh at the age of 4 months of a calf. The mesh was anchored subcutaneously to strong supportive musculature with interrupted pattern using No. 2 catgut sutures. polypropylene mesh proved alternative for hernial repair when fixed subcutaneous in large hernial ring in male and female calves without complications. Therefore, prosthetic mesh represents a safely procedure in large hernial ring to avoid over-stretching on the edges of the wound which hinders wound healing. The present case report discusses the successful management of umbilical hernia in crossbred female calf.
Keywords: Crossbred female calf, Umbilical hernia, Surgery, Polypropylene mesh, Uneventful recovery
Introduction
A hernia is a protrusion of the contents of a body cavity through a weak spot of the body wall. This may be from accidental or a normal anatomical opening, which does not completely fulfill its physiological function. It is a common defect in calves (Rings, 1995 ). Congenital umbilical hernias are of concern for heritability. Multiple births and shortened gestation lengths are two important risk factors for congenital umbilical hernias in calves. In the past, hernial surgery and abdominal wall reconstructions frequently have used tense suture to approximate and close a hernial ring or defect. Large hernia requires safe closure to avoid wound dehiscence, recurrent hernias and no healing of the wound due to tissue ischemia with the sutures cutting through the soft tissue (Matthews et al., 2003).The successful repair of an abdominal wall defect is based on a tension-free closure to allow wound repair, a better collagen restoration and prevention of recurrence. Polypropylene mesh is strong, has excellent tissue incorporation, and is relatively inexpensive.. Simple apposition of hernial ring with minimal or complete avoidance of tension at the healing suture line is essential for ideal healing (Mc Farland,1980 and Fubini and Ducharme, 2004).This may not be possible for hernias with large ring, unless the use of prosthesis is employed. The mesh helps in reducing recurrent rate of hernia and also allows faster recovery. Correction of hernia could simply be done by suturing the body tissues (Herniorraphy) or by implantation of foreign materials to give a greater strength (Hernioplasty).Choice of suitable technique to be employed depends on the size of the hernial ring. When a large defect makes the approximation of tissues impossible without undue tension, prosthetic implants are used and the most commonly used synthetic material is a mono-filament plastic mesh made of polypropylene or polyethylene (Zimmerman, 1968).
Materials and Methods
The calf was prepared routinely for aseptic surgery after a preoperative fasting for 24 hours. The calf was physically controlled in dorsal recumbancy.Xylazine hydrochloride was used as sedative in dose of 0.1mg/kg body weight intra muscular. Local infiltration anesthesia using 7-10 ml of 2% Lidocaine hydrochloride was infiltrated subcutaneously around the swelling in ring block. An elliptical skin incision was made over the external hernial sac was made. The internal hernial sac was bluntly dissected and freed down to the hernial ring . After reduction of the hernial contents, the hernial ring was repaired with polypropylene mesh using mattress suture pattern. The mesh extended 1.5 – 3 cm beyond the margins of the defect and is anchored subcutaneously to strong supportive structures with interrupted sutures (Fig1.3) Fixing of the prosthetic mesh in musculature was realized using No.2catgut sutures in simple interrupted patterns, Application of sutures was made under fingers protection, avoiding puncture of the bowel. The subcutaneous tissue was mobilized and sutured above the mesh, using No. 2 catgut. The skin was closed by interrupted patterns using cotton thread. Postoperative care consisted of administration of flunixin meglumine as a nonsteroidal anti inflammatory as 1.1 mg/kg body weight given IM in addition to streptopenicilline as 1mg / 25kg body weight given IM. Daily dressing of suture line with 5% povidone iodine. The skin sutures were removed after 15 days postoperative depending upon the wound condition.
Results and Discussion
Fixing of the polypropylene mesh outside the abdominal wall defect, using interrupted mattress sutures was easier and proved effective in closing the ring. Minor post surgical complications were observed after 2-3 days in form of inflammatory swelling in navel region. They were completely subsided within 2 weeks with the usage of antibiotics and non-steroidal anti inflammatory. Healing was achieved in good condition. treated calf recovered without major complications or recurrence. A tension free mesh technique has drastically reduced recurrence rates for all hernias compared to tissue repairs and has made it possible to reconstruct large ventral defects that were previously irreparable. Placement of the polypropylene mesh outside of the abdominal wall in subcutaneous position was preferable. The fixation was easier and their was no complications similar to the findings of Vander Velden and Klein (1994) for placing the polypropylene mesh outside of abdominal wall defect because the mesh being placed superficially. This fixation ensured preventing the most important complications induced by the contact of prosthetic meshes of polypropylene and abdominal bowels, formation of adhesions and fistulas (Matthews et al., 2003).




Conclusion
Accordingly, an umbilical hernia can be well managed through hernioplasty using polypropylene mesh where hernial ring size is more than 5 cms , recommended as an alternative technique. Sharing pics of the same calf after 2 years of surgery given a birth to a healthy female calf.
References
- Bellas P., 1987. Contribution á l’ étude du “gros nombril” du veau. Cure chirurgicale par pose d’une crinoplaque, Thèse de doctorat vétérinaire, Lyon.
- Elce Y.A., Kraus B.M., Orsini J.A., 2005. Mesh hernioplasty for repair of incisional hernias of the ventral body wall in large horses, Equine vet. Educ. 17 (5): 252-256.
- Freeman D.E., 2005. Management of ventral incisional hernias in large horses: a surgical challenge, Equine vet. Educ.17 (5): 247-251.
- Fubini, S., Ducharme, N.G., 2004. Surgical Management of Umbilical Hernia; Food Animal Surgery, Saunder Publication, an imprint of Elsevier Sciences, Philadelphia, United States of America. Pp.: 482-484.
- Herrmann, R., Utz, J., Rosenberger E., Wanke R., Doll, K., Distl O., 2000. Investigations on occurrence of congenital umbilical hernia in German Fleckvieh. Zuchtungskunde. 72, 258- 273.
- Matthews, B.D., Pratt B.L., Pollinger H.S., Backus C.L., Kercher, K.W., Sing R.F., Heniford B.T. 2003. Assessment of adhesion formation to intra-abdominal polypropylene mesh and polytetrafluoroethylene mesh. J. Surg. Res. 114 (2): 126-132.
- Mc Farland, J. 1980. Hernia: Basic Clinical Surgery for Nurses and Medical Students. 2nd Edition. Butterworth and Co. (Publishers) Ltd, London, United Kingdom. Pp.: 580-589.
- Müller, W., Schlegel, F., Haase, H., Haase G., 1988. Zum angeborenen Nabelbruch beim kalb. Monatshefte für Veterinärmedizin. 43, 161-163.
- Rings, D.M. 1995. Umbilical hernias, umbilical abscesses, and urachal fistulas. Surgical considerations. Vet. Clin. North Am. Food Anim. Pract. 11:137–148.
- Steenholdt, C., Hernandez J., 2004. Risk factors for umbilical hernia in Holstein heifers during the first two months after birth. J. Am. Vet. Med. Assoc. 224:1487– 1490.
- Tulleners, E.P., Fretz P.B. 1983. Prosthetic repair of large abdominal walldefects in horses and food animals, J. Am. vet. Med. Ass. 182: 258-262.
- Usher, F.C. 1959. A new plastic prosthesis for repairing tissue defects of the chest and abdominal wall, Am. J. Surg. 97: 629–263.
- Usher, F.C.1970. The repair of incisional and inguinal hernias, Surg. Gynecol. Obstet. 1: 525–530.
- Van der Velden, M.A. Klein, W.R. 1994. A modified technique for implantation of polypropylene mesh for the repair of external abdominal hernias in horses: a review of 21 cases, Vet Q. 2: 108-110.
- White, N.A. 1996. Incisional hernia after abdominal surgery in the horse. Equine vet. Educ.; 8: 308-312.
- Wilhelm, T.J., Freudenberg, S., Jonas, E., Grobholz R., Post, S. Kyamanywa, P., 2007. Sterilized mosquito net versus commercial mesh for hernia repair; an experimental study in Mbarara/Uganda. Eur. Surg. Res. 39 (5): 312-317.
- Zimmerman, L.M., 1968. The use of prosthetic material in the repair of hernia. In: Slatter, D. (Ed). Textbook of Small Animal Surgery. 3rd Edition, Volume 1. An imprint of Elsevier Science. Saunders Publishers, United States of America. Pp.: 44.
| The content of the articles are accurate and true to the best of the author’s knowledge. It is not meant to substitute for diagnosis, prognosis, treatment, prescription, or formal and individualized advice from a veterinary medical professional. Animals exhibiting signs and symptoms of distress should be seen by a veterinarian immediately. |





Be the first to comment