According to the Ministry of statistics and programme implementation, 2020, the current population of India is close to 1.380 billion or 1,380 million or 138 croreswith second most populous countries in the world behind China.While the overall literacy rate is 64.8 % which suggest almost half population is still uneducated. We can estimate how many people out of 64.8 % educated lot would know about AMR. Probably less than 1% which includes the people involve in medical field or research field.Even single person of India played role for increased AMR in past decayed by increased use of antibiotics in daily basis. India is the leading antibiotic consumer in the world with 12.9×109 unit’s consumption every year, closely followed by China at 10.0×109 units and the USA at 6.8×109 units.
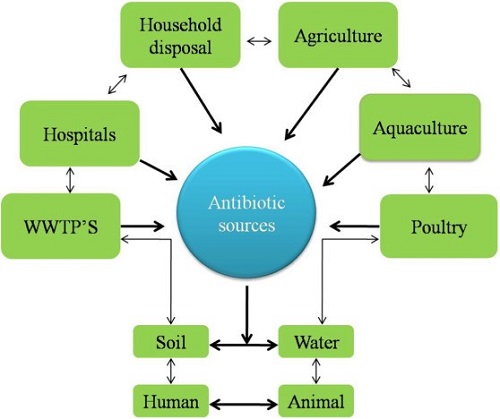
Antimicrobial resistance (AMR) may be responsible for approximately 90% of the predicted deaths to occur in Asia and Africa by 2050.Figure.1 is predicting the source of antibiotic responsible for Antibiotic resistance.Antibiotics have been sold like sweets because people think antibiotics are the only solution for their health problems, as a results India become has emerged as a global hotspot for antibiotic resistance (ABR). All we need to aware the population or prove that antibiotics also work on ALL or NONE phenomenon.
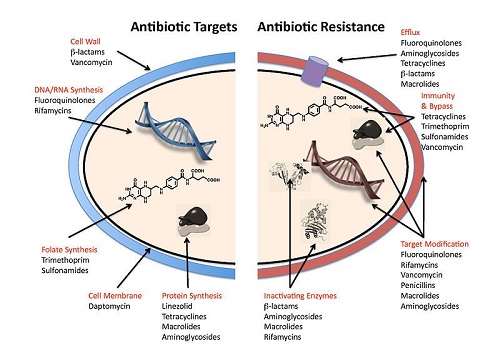
All or None phenomenon is generally applicable in case of human nerve or muscle fiber. According to that phenomenon the strength of a response of a nerve cell or muscle fibres is not dependent upon the strength of the stimulus. If a stimulus is above a certain threshold, a nerve or muscle fibres will fire. It means no response beyond threshold level same as in case of overuse or unnecessary use of antibiotics. Infections or diseased caused by different bacteria i.e. E.coli, K. pneumoniae can be cured by use of antibiotics but with the time bacteria also evolved so many methods to resist effect of these antibiotics. Figure 2 shows representing the different method of resistance.
Several factors are responsible for increased antibacterial resistance. The important factors include
- Lack of appropriate knowledge
- Overuse of antibiotics
- Desired to meet patient demand
- Extensive agricultural use
- Economic incentives
- Marketing influence
- Traditional beliefs about antibiotics
- Lack of transparency in the global pharmaceutical supply chain.
- Discharging pharmaceutical effluent into the environment
Antibiotics are being used in almost every field that’s the only cause behind transformation of antibiotics from all to none phenomenon. India is primarily agriculturally based country. Approximatelly 70 % of population is working for fulfillment of their basic needs like food. If we concerned only up to the food antibiotics are used in meat and milk industries and others also. In food animal’s antibiotics are used for the purpose of prevention, control and treatment of disease as well as for growth promotion.
Organization for economic cooperation and development (OECD) estimates antimicrobial use in food animal globally from 63,151 tons in 2010 to 105,596 tons by 2030 – an increase of 67%. 45mg of antimicrobials are used to produce 1kg of beef.148mg of antimicrobials are used to produce 1kg of chicken.172mg of antimicrobials are used to produce 1kg of pork. Table 1 represents the percentage of AMR in different types of food.
| Sr. No | Type of sample | Antibiotic used | Antimicrobial resistance |
| 1. | Poultry meat | Penicillin, Ampicillin | 89.4%, 80.43 % |
| 2. | Fruits, vegetable | Multidrug resistant | 61.1 % |
| 3. | Chicken sample | Ampicillin, Enrofloxacin | 62.5 %, 87.5 % |
| 4. | Feed, Meat and bone meal | Ciprofloxacin, Enrofloxacin | 100 %, 90 % |
| 5. | Meat sample | Trimethoprim, Ampicillin | 50 %, 20%. |
| 6. | Chevon, chicken meat | Erythromycin,MDR | 93.75%, 43.75 % |
| 7. | Bovine milk | Amikacin, Azithromycin | 58.3%, 41% |
| 8. | Chicken, chevon | Oxytetracycline, Ampicillin | 34.03%, 29.31% |
| 9. | Chicken samples | Cefotaxime, Ciprofloxacin | 100%, 83% |
| 10. | Beef samples | Amoxicillin, Tetracycline | 28.8%, 24.4% |
Table 1: Antimicrobial resistance in food
Ground water sites and a large proportion of aquatic antibiotic contamination is due to human antibiotic usage, i.e., hospital effluents and municipal sewage and wastewater which eventually ends up in the environment. Increased resistance towards antibiotics will impact human, animal as well as environment which results in increased human morbidity and mortality, reduced antibiotic efficiency and increased carriage and dissemination.
Veterinary antibiotics soil concentrations reaching as high as 9,990ug kg -1. Different antibiotics residue is present in water bodies like Macrolides, sulfonamides, tetracycline, chloramphenicol, chlortetracycline, sulfamethazine, lincomycin, trimethoprimand sulfamethazine. Veterinary and human antibiotic sulfamethoxazole was found in 23% of the 47%. To combat AMR the only option left for India is to give emphases on stewardship programme and to follow the rules and regulations provided by government.
Regulations on antibiotic use in food producing animals:
- Food Safety and Standards (Contaminants, Toxins and Residues) Amendment Regulation (2017): States that for a list of 21 antibiotics the tolerance limit, used in human beings and animals will be 0.01mg/kg.
- MPEDA’s: 20 antibiotics and pharmacologically active substances banned for use in aquaculture include Chloramphenicol, Nitrofurans etc.
- WHO’s list of Critically Important Antimicrobials important for human health and should be restricted in the veterinary sector include: Ampicillin, amoxycillin, cefadroxil, chlortetracycline, doxycycline, erythromycin, flumequine, gentamycin, veneomycin, oxytetracycline, spiramycin, sulfadiazine.
For veterinary practitioners:
- Prescription should be based on clinical diagnosis and after conducting sensitivity test.
- Practitioners should avoid metaphylaxis antibiotics and increase good veterinary and husbandry practices.
- They should prefer narrow-spectrum antibiotics as their first choice (broad spectrum avoid) with scientific based antibiotic therapy.
- Combined therapy with synergic drugs (MDR) should be applied together to minimize or reduce the need to veterinary antibiotics with appropriate dose, route and duration of antibiotics.
- Other than this effective research with awareness and education among public is strong weapon for antimicrobial resistance.
| The content of the articles are accurate and true to the best of the author’s knowledge. It is not meant to substitute for diagnosis, prognosis, treatment, prescription, or formal and individualized advice from a veterinary medical professional. Animals exhibiting signs and symptoms of distress should be seen by a veterinarian immediately. |





Be the first to comment