Abstract
Coronavirus disease is the recent cause of global concern. The massive outbreak of COVID-19 has led the World Health Organization (WHO) to declare this as a pandemic situation. COVID19 is caused by the SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus-2), which causes severe respiratory illness and death in humans. The first laboratory diagnosis of SARS-CoV-2 in a pet dog in Hong Kong, suggests that the virus is zooanthroponotic, implying that it can be transmitted from human to animal. Thereafter, many animals including mink, lion, tiger, cat have also been reported to acquire the virus in several countries. In this situation, the veterinarian’s role is crucial in treating the animals, helping in food security, disease diagnosis, surveillance, and boosting the the economy of livestock stakeholders at the grass-root level. Despite the lack of specific antiviral drugs against SARS-CoV-2 and suitable vaccine candidates in pre-clinical and clinical trials, a global vaccination drive against SARS-CoV-2 has started to anticipate triumph over this pandemic with a collaborative, multisectoral, and transdisciplinary strategy connecting human, animal, and environmental health. This article explores the role of veterinarians in managing and protecting public health to pave the way for the implementation of a one-health approach to biodiversity conservation.
Keywords: COVID-19, Veterinarian, WHO, Animals, Humans, Pandemic.
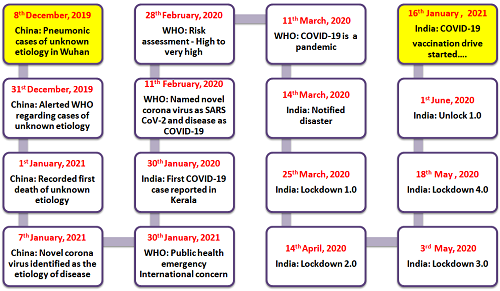
Introduction
The current global population is experiencing the worst of its medical emergency as every individual is either directly or indirectly fighting against the emerging pandemic COVID-19. Coronaviruses (CoVs) are well-known causes of serious infections in humans and a variety of animal hosts, including horses, cattle, camels, cats, swine, rodents, dogs, mink, bats, palm civets, rabbits, ferrets, snakes, avian species, and wild animals. (Fehr and Perlman, 2015). In Wuhan, China, several cases of Viral Pneumonia with Unknown Etiology (VPUE) were reported. These patients presented with clinical symptoms of fever, dry cough, dyspnea, and bilateral lung infiltrates on imaging. Many of the cases are linked to Wuhan’s Seafood Wholesale Market, which deals with fish and other live animals like poultry, marmots, bats, and snakes. The pandemic caused by a new corona virus (CoV) was named earlier as 2019 novel Corona virus (2019-nCoV) (Schwegmann-Wessels and Herrler, 2006) but later, on February 11th 2020, its new nomenclature was formulated by the Corona virus Study Group (CSG) of International Committee on Taxonomy of Viruses (ICTV) as “Severe Acute Respiratory Syndrome Corona virus 2 (SARS-CoV-2)” and the disease was termed as “COVID-19” (Peeri et al., 2020). The World Health Organization affirmed the spread as a global pandemic. As of March 26th 2021, WHO had received reports of 124,871,140 confirmed COVID-19 cases worldwide, including 2,744,543 deaths. In India, there have been 11,846,652 confirmed cases and 1, 60,949 deaths.
Virology
Corona viruses (CoVs) are the largest family of viruses found in nature. CoVs are members of the Coronaviridae family and the Nidovirales order, with a single-stranded, positive-sense RNA genome and the size ranges from 26 to 32 kb (the largest genome of known RNA viruses). The Orthocoronavirinae subfamily is classified into four genera based on genome structure and phylogenetic analysis: namely, Alphacoronavirus, Betacoronavirus, Gammacoronavirus, and Deltacoronavirus. Only Alphacoronavirus and Betacoronavirus infect mammals and cause respiratory infections in humans and enteritis in animals. SARS-CoV and MERS-CoV are two major zoonotic pathogenic corona viruses of the genus Betacoronavirus. The Betacoronavirus is divided into five subgenera, among which, Sarbecovirus, contains SARS-CoV and the novel corona virus (2019-nCoV) (Ghelichi-Ghojogh et al. 2020). Hibecovirus, Embecovirus, Nobecovirus, and Merbecovirus are the other subgenera of Betacoronavirus.
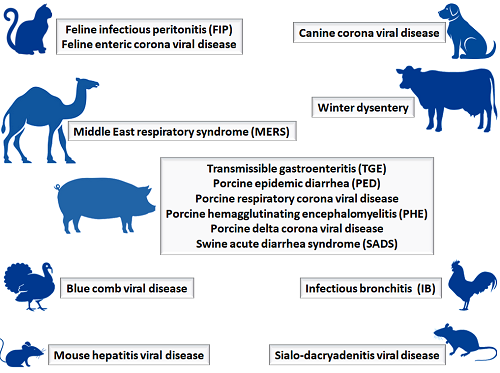
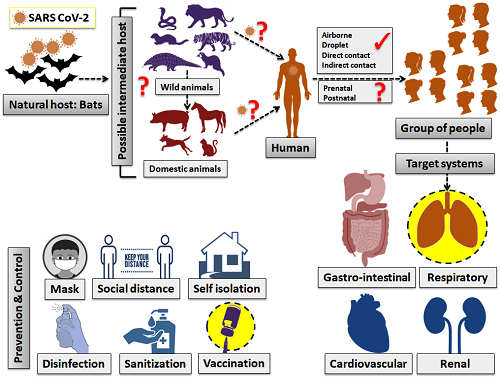
Host range
Corona viruses (CoVs) infect humans as well as wild and domestic animal species, and most infections are subclinical (Padenet al., 2018). Cattle, horses, cats, dogs, pigs, camels, rabbits, birds, rodents, mink, ferrets, snakes, bats, hedgehogs, frogs, marmots, pangolins, as well as other wild animals have been recorded to harbor CoVs, and their role as carrier/reservoir is of crucial importance. (Dhama et al. 2020). The clinical form varies from enteritis in cattle, swine, and horses, upper respiratory tract infections in dogs, cattle, felines, and poultry. In humans, from a common cold to potentially fatal respiratory infections may be found. (Salata et al. 2020; Dhama et al., 2020). Bats are perfect reservoir hosts for CoVs, as viruses are steadily present in bats and being asymptomatic. In the current COVID-19 pandemic, laboratory findings confirmed that SARS CoV-2 is also 96% identical to the bat CoV at the genomic level, and hence bats may be the primary source of this zoonotic spillover (Millán-Oñate et al. 2020). Coronavirus has been isolated not only from bats, but also from Malayan Pangolins, and receptor-binding domain (RBD) in S protein of SARS-CoV-2 was relatively similar to that of Pangolin-CoV, indicating that pangolins could be the intermediate host of SARS-CoV-2. (Xiao et al. 2020). Till now, SARS-CoV-2 infection has been noticed in two dogs (Shi et al. 2020). Of late, a Malayan tiger maintained in the Bronx Zoo of New York City, NY, USA was also tested positive for SARS-CoV-2 (Ahmad et al., 2020). Supplementary studies are mandatory to spot the intermediate host and to prove their role in the origin of SARS-CoV-2 in humans.
Transmission
SARS-CoV 2 is chiefly transmitted from symptomatic people to others who are in close contact through respiratory droplets, by direct contact with infected persons, or by contact with contaminated objects and surfaces (Jiang et al., 2020). SARS-CoV 2 possibly will transmit through the animals such as pig, cat, dog, cow, and turkeys. As a precaution, avoid contact and isolate them if any infection signs such as diarrhea, cold, fever are detected. COVID-19 transmission is classified into four stages, according to the WHO. Some countries or regions have the following characteristics: 1. There have been no recorded incidents. 2. Situations that occur infrequently 3. Case clusters (grouped by location and time), or 4. Community transmission As per WHO and ECDC guidelines avoid contact with the sick person and also pass up the market or public place as per possible (Daszak et al., 2020).
Clinical symptoms
COVID-19 has a wide variety of clinical symptoms, ranging from symptomless to acute respiratory distress syndrome (ARDS) and multi-organ failure. (Wang et al., 2020). The common clinical features include anorexia, fever, dry cough, diarrhea, sore throat, fatigue, headache, myalgia, and breathlessness (Cui et al., 2019). Thus, they are impossible to differentiate from other respiratory infections. Individuals with a high level of comorbidity are predisposed to severe infection and can often present with acute kidney injury (AKI) and ARDS symptoms (Huang et al., 2019). In some patients, the disease will lead to pneumonia, respiratory failure, and death by the end of the first week. This sequence is linked with a tremendous rise in inflammatory cytokines (cytokine shower) including IL2, IL7, IL10, GCSF, IP10, MCP1, MIP1A, and TNFα (Wang et al., 2020).
Pathophysiology
SARS-CoV-2 has a structure typical to other corona viruses, and its genome has been compared to a previously reported coronavirus strain that caused the SARS outbreak in 2003 (Lu et al., 2020). SARS corona virus (SARS-CoV) has a well-defined structural composition that includes 14 binding residues that interact directly with human angiotensin-converting enzyme 2. (ACE 2) (Wiersinga et al., 2020). In SARS-CoV-2, eight of these amino acids have been conserved. (Fehr et al., 2015). Before the identification of SARS-CoV and MERS corona viruses, corona viruses were believed to cause only minor respiratory infections in humans (MERS-CoV) (Bourgonje et al., 2020). While the precise pathophysiological mechanisms behind the emergence of SARS-CoV-2 remain unclear (due to pending laboratory trials), genomic similarities to SARS-CoV may help to understand the inflammatory reaction that can lead to severe pneumonia (Olwenyi et al., 2020). The exact mechanism of SARS-CoV-2 will remain unknown until these laboratory trials begin.
Diagnosis
The chest X-ray (CXR) in humans normally reveals bilateral infiltrates, although it can be normal in the early stages of the disease. The CT scan is more accurate and sensitive. Infiltrates, ground-glass opacities, and subsegmental consolidation are commonly seen on CT imaging. (Littrup et al., 2005; Beck et al., 2020). Broad laboratory tests should be requested for patients with suspected infection. Patients may have elevated C-reactive protein, lactate dehydrogenase, erythrocyte sedimentation rate, and a prolonged prothrombin time (Bai et al., 2020). Usually, the white cell count is normal or minimal. Lymphopenia is possible; a lymphocyte count of <1000 has been related to serious disease. In most cases, the platelet count is normal or slightly low. A high level of procalcitonin could suggest bacterial co-infection. High levels of ALT/AST, creatinine, prothrombin time, CPK, D-dimer, and LDH are associated with severe disease (Zhu et al., 2019). In all the confirmed veterinary cases of SARS-CoV-2, the samples collected for examination were either vomit, rectal swab, nasal swab, or feces. Most of the laboratory confirmation was by real-time reverse transcriptase-polymerase chain reaction (RT-PCR) mostly targeting the N gene of virus and few by next-generation sequencing (NGS) of viral DNA (Huang et al., 2020).
Differential diagnosis
The differential diagnosis covers all forms of respiratory viral infections (Influenza, Human Metapneumovirus, Respiratory Syncytial Virus (RSV), Parainfluenza, Adenovirus), atypical species (Chlamydia, Mycoplasma), and bacterial infections. (Fang et al., 2020). It is not possible to differentiate COVID-19 from these infections clinically or through routine lab tests. In these instances, the RT-PCR assay and NGS would be used for confirmation (Hong et al., 2020). Therefore travel history becomes important. However, as the epidemic spreads, travel history will become irrelevant.
Roles and responsibilities of the veterinarians in the one health
As a precautionary measure to combat the pandemic, several countries have imposed lockdown. Today, only a few important services are available to the public, including emergency services to maintain animal well-being and safety. Veterinary doctors work with livestock, pets, birds, and wild animals to diagnose, cure, and avoid diseases.
- They also assist with the planning of vaccines and deworming camps. Apart from that, they also have many important tasks to fulfill. We would like to shed some light on the programs that veterinarians should participate to combat COVID-19. Human sample processing and screening can be done in laboratories by veterinary microbiologists and biotechnologists who have been trained and appointed.
- Aside from protecting livestock by preventing diseases and zoonoses, veterinary epidemiologists may recommend surveillance strategies based on their previous encounters with animal epidemics (avian influenza, rinderpest, bluetongue, and so on).
- SARS-CoV-2 transmission via food intake has yet to be proven. However, given the public’s apprehension of contracting COVID-19 from animal food intake, proper food processing, and inspection are critical.
- Heparan sulfate, a negatively charged glycosaminoglycan found in animal meat, is thought to be a suitable anchor for the spike protein of SARS-CoV-2. As a result, veterinarians should thoroughly test animal food and educate the public about their fears, which may have major epidemiological implications, to ensure the food chain’s safety.
- Furthermore, veterinarians must pay special attention to the management of zoo animals and endangered wildlife, since the disease has already been documented in tigers and lions.
- In the case of livestock owners, a veterinarian will assist them in raising livestock and maintaining farms, reopening a source of income for the unemployed, and restoring the country’s economy.
- Ferrets and hamsters are two animal models recently proposed by the OIE for evaluating vaccines and drugs against SARS-CoV-2, so veterinarians play a key role in determining vaccine safety in animal models.
- Veterinarians should be prioritized in all of these areas, from laboratory/experimental animal control to designing animal models for virus pathogenesis research to vaccine trials.
- Apart from the above, veterinary researchers may be appointed to manufacture human vaccines because they are well-versed in cutting-edge health-related molecular techniques.
- A rise in the number of SARS-CoV-2 cases in animals has been recorded, requiring more research to improve vaccines and testing kits for susceptible animals.
- Many veterinary colleges and research institutes are currently involved in the processing and screening of human samples for SARS-CoV-2 using biosafety level -3 (BSL-3) and real-time PCR devices.
- As the world continues to be perplexed about the reservoir of SARS-CoV-2, further testing and monitoring by veterinarians are needed to determine the true origin of the diseases.
- We should provide a barrier between the reservoir and humans with the aid of a veterinarian as a precaution to avoid further outbreaks.
- Human vaccinations and antiviral medicines can be produced in large amounts by veterinary vaccine makers and pharmaceutical companies, respectively.
- Finally, but certainly not least, veterinarian hospitals will support medical health facilities by contributing critical items like personal protective devices and ventilators.
Treatment
Currently, no effective antiviral treatment available for COVID-19. On the other hand, a randomized multicenter controlled clinical trial is currently being conducted to evaluate the effectiveness and safety of COVID-19 in patients. Antipyretic medicine, such as paracetamol, is the first-line treatment for fevers, while expectorants, such as guaifenesin, can be used to relieve a nonproductive cough. (Bai et al., 2020). Patients with a severe acute respiratory illness, hypoxemia, respiratory distress, or shock need to get oxygen treatment right away. Intravenous fluids should be carefully administered in the absence of shock. (Schultz et al., 2017). Patients with AKI should begin renal replacement therapy (RRT) immediately. Within the first hour after being diagnosed with sepsis, broad-spectrum antibiotic therapy should be started (Rhodes et al., 2017). Patients can develop new bacterial and fungal infections during the middle and late stages of the disease. Therefore, antibiotic regimens that are conservative and rational must also be used (Liu et al., 2020). Glucocorticoids may also be considered for patients with severe immune reactions.
Table 1: List of few candidate vaccines developed against SARS-CoV 2 in the preclinical and clinical trial
| S.No | Vaccines | Mechanism | Developer |
| 1 | Covishield | Non-replicating viral vector | Oxford University / Astra Zeneca / SII |
| 2 | Covaxin | Whole-cell Inactivated vaccine | Bharat biotech / NIV |
| 3 | NVX-CoV | Protein subunit | Novavax |
| 4 | ZyCov-D | Plasmid DNA vaccine | Zyduscadilla |
| 5 | Janssen COVID-19 | Non-replicating viral vector | Johnson and Johnson |
| 6 | Gamaleya (Sputnik V) | Non-replicating viral vector | Dr.Reddys |
| 7 | Moderna | m RNA based vaccine | BARDA / NIAID |
| 8 | Pfizer-BioNtech Covid 19 | m RNA based vaccine | Pfizer-BioNtech |
(SII-Serum Institute of India; NIV-National Institute of Virology; BARDA-Biomedical Advanced Research and Development Authority; NIAID-National Institute of Allergy and Infectious Disease)
Prevention and Control
- Since few cases of human-to-animal transmission of SARS-CoV-2 have been recorded in many countries, veterinary personnel with feverish or other symptoms of COVID-19 should not treat the animal.
- In the event of a veterinary emergency, a sick veterinarian should take all necessary precautions to avoid disease transmission.
- To reduce the number of visits to polyclinics, the government should legalize and encourage veterinary telemedicine facilities in the region.
- Before starting care, the staff can take down the patient’s contact information as well as the owner’s epidemiological background.
- Every public and private veterinary hospital should have an isolation room or space to deal with both suspected and confirmed patients.
- After this, veterinarians should thoroughly examine the spread of the Virus to different organs for the autopsy of either naturally or experimentally infected animals to find potential ways of shedding viruses by animals.
- The virus was found in urine or vomit from sick animals. so animal monitoring is important in the field in which the dissemination of community is apparent.
- Suitable precautions in the treatment of veterinarians and staff should be taken in the treatment of the patient with the donning and doffing of personal protective equipment (PPE).
- Veterinarians shall stick exclusively to the biosafety and biosafety steps throughout the treatment of every patient.
- Veterinary surgeons working in the pandemic shall be kept up to date with all guidelines developed by the Department of Animal Husbandry in every country as well as the OIE.
- Veterinarians should be solely responsible for alerting farm operators, pet owners, and staff at the grassroots level.
- The principle of one health should be introduced globally in the future as a veterinarian plays a vital role in maintained stable and human and animal welfare environments, thus reducing economic effects on animal and food production.
- Because of their high susceptibility, risk assessments for the Felidae family (tigers, jaguars, lions, cougars, cheetahs, and leopards), as well as great apes ( gorillas, chimpanzees, and orangutans), are needed.
- Rapid detection, close caution, adequate isolation, and quarantine protocols are all being used to monitor the spread of this new virus.
- Enhanced oversight and monitoring, as well as the upgrading of emergency departments and intensive care units, networking programs, accelerated coordination and information sharing, and improved public knowledge of the risks to all general public are all on the agenda.
- International collaboration and preparedness to tackle further emergency that has the potential to become a heightened pandemic.
- Strengthening one health solution to fight this new virus that causes wreaking havoc on the lives of billions of people has to be implemented successfully (Bonilla-Aldana et al., 2020).
- In the form of vaccines, the COVID-19 pandemic seems to have a long-term solution. There are currently no authorized and safe vaccines against it (Chen et al. 2020), but suitable vaccine candidates are still being investigated in preclinical and clinical vaccine trials. Despite this, almost all countries have begun vaccine drive to tackle the wreaking havoc posed by SARS-CoV-2.
Conclusion
The source of SARS-CoV-2 infection in human has not been undoubtedly recognized so far, though the human-to-animal transmission has been well observed in all the reported cases and thus may allege the disease as anthroponosis in near future. Therefore there may be a surge in the asymptomatic reservoirs and carriers of the virus in the environment that may perhaps minimize the ability to limit the spread of this pandemic. In these circumstances, many important aspects like food safety, disease diagnosis, prevention of outbreaks in humans and animals, and safeguarding public health, etc. play fundamental roles in our society and the taking on suitable public health preventive actions and intensification of medical facilities are the best options for administrating the disease. This can only be achieved fruitfully by including veterinarians in the global health system during this pandemic. Concerning animal health, companion animals of COVD-19 infected owners should be quarantined and may be recommended for screening for the presence of the virus. All zookeepers should be scanned for the disease before contacting the zoo animals. Army dogs are the most exclusive and are also an integral part of the country’s security, hence their surveillance is the greatest importance. The veterinary branch of all territories should take the responsibility of reporting the detailed information of all confirmed cases of animals to OIE within the earliest time. To combat this pandemic, the country’s legislation should act vigorously considering the “One Health” approach to conserve biodiversity by acting synchronously towards the welfare of human and animal health combinedly.
References
- Almendros, A., 2020. Can companion animals become infected with Covid-19?. Veterinary Record, 186(12), pp.388-389.
- Bai, Y., Yao, L., Wei, T., Tian, F., Jin, D.Y., Chen, L. and Wang, M., 2020. Presumed asymptomatic carrier transmission of COVID-19. Jama, 323(14), pp.1406-1407.
- Beck, M. and Tobin, D., 2020. The 2019/2020 Novel Corona virus outbreak: an International health management Perspective. The Open Public Health Journal, 13(1).
- Benvenuto, D., Giovanetti, M., Ciccozzi, A., Spoto, S., Angeletti, S. and Ciccozzi, M., 2020. The 2019‐new coronavirus epidemic: evidence for virus evolution. Journal of medical virology, 92(4), pp.455-459.
- Bonilla-Aldana, D.K., Dhama, K. and Rodriguez-Morales, A.J., 2020. Revisiting the one health approach in the context of COVID-19: a look into the ecology of this emerging disease. Adv Anim Vet Sci, 8(3), pp.234-7.
- Businessweek, B., 2020. Coronavirus Is More Dangerous for the Global Economy Than SARS
- Chen, J., 2020. Pathogenicity and transmissibility of 2019-nCoV—a quick overview and comparison with other emerging viruses. Microbes and infection, 22(2), pp.69-71.
- Chen, L., Zhou, M., Dong, X., Qu, J. and Gong, F.Y., 2001. han Y. Yang F, Zhang tJ.
- Chen, N., Zhou, M., Dong, X., Qu, J., Gong, F., Han, Y., Qiu, Y., Wang, J., Liu, Y., Wei, Y. and Yu, T., 2020. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. The lancet, 395(10223), pp.507-513.
- Chu, C.M., Cheng, V.C.C., Hung, I.F.N., Wong, M.M.L., Chan, K.H., Chan, K.S., Kao, R.Y.T., Poon, L.L.M., Wong, C.L.P., Guan, Y. and Peiris, J.S.M., 2004. Role of lopinavir/ritonavir in the treatment of SARS: initial virological and clinical findings. Thorax, 59(3), pp.252-256.
- Cui, J., Li, F. and Shi, Z.L., 2019. Origin and evolution of pathogenic coronaviruses. Nature Reviews Microbiology, 17(3), pp.181-192.
- Daszak, P., Olival, K.J. and Li, H., 2020. A strategy to prevent future epidemics similar to the 2019-nCoV outbreak.
- Dhama, K., Patel, S.K., Sharun, K., Pathak, M., Tiwari, R., Yatoo, M.I., Malik, Y.S., Sah, R., Rabaan, A.A., Panwar, P.K. and Singh, K.P., 2020. SARS-CoV-2: Jumping the species barrier, lessons from SARS and MERS, its zoonotic spillover, transmission to humans, preventive and control measures and recent developments to counter this pandemic virus.
- Fehr, A.R., HJ, P.S.M., Bickerton, E. and Britton, P., 2015. An Overview of Their Replication and Pathogenesis; Section 2 Genomic Organization. Methods in Molecular Biology. Springer, 1282, pp.1-23.
- Food and Agriculture Organization of the United Nations/World Health Organization (FAO/WHO). 2008.Microbiological hazards in fresh leafy vegetables andherbs: meeting report. Microbiological Risk AssessmentSeries No. 14. Rome. 151.
- Ghelichi-Ghojogh, M., Allah Kalteh, E. and Fararooei, M., 2020. Coronavirus disease 2019; epidemiology and recommendations. J Prev Epidemiol, 5(1), p.e01.
- https://covid19.www.who.int/emergencies/diseases/novel-coronavirus-2019
- Huang, C., Wang, Y., Li, X., Ren, L., Zhao, J., Hu, Y., Zhang, L., Fan, G., Xu, J., Gu, X. and Cheng, Z., 2020. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The lancet, 395(10223), pp.497-506.
- Jiang, R.D., Liu, M.Q., Chen, Y., Shan, C., Zhou, Y.W., Shen, X.R., Li, Q., Zhang, L., Zhu, Y., Si, H.R. and Wang, Q., 2020. Pathogenesis of SARS-CoV-2 in transgenic mice expressing human angiotensin-converting enzyme 2. Cell, 182(1), pp.50-58.
- John, S.D., 2009. „Supreme Emergencies, Epistemic Murkiness and Epistemic Transparency”. Philosophy of Management. 1 aprilie 2009.
- Kebede, A., Review of Emergence and Zoonotic Implication of Sars-Cov-2 (Covd 19) and its Associated Risk Factors.
- Lau, S.K., Lau, C.C., Chan, K.H., Li, C.P., Chen, H., Jin, D.Y., Chan, J.F., Woo, P.C. and Yuen, K.Y., 2013. Delayed induction of proinflammatory cytokines and suppression of innate antiviral response by the novel Middle East respiratory syndrome coronavirus: implications for pathogenesis and treatment. Journal of General Virology, 94(12), pp.2679-2690.
- Littrup, P.J., Freeman-Gibb, L., Andea, A., White, M., Amerikia, K.C., Bouwman, D., Harb, T. and Sakr, W., 2005. Cryotherapy for breast fibroadenomas. Radiology, 234(1), pp.63-72.
- Liu, K., Fang, Y.Y., Deng, Y., Liu, W., Wang, M.F., Ma, J.P., Xiao, W., Wang, Y.N., Zhong, M.H., Li, C.H. and Li, G.C., 2020. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chinese medical journal.
- Lu, H., Stratton, C.W. and Tang, Y.W., 2020. Outbreak of pneumonia of unknown etiology in Wuhan, China: the mystery and the miracle. Journal of medical virology, 92(4), pp.401-402.
- Lu, R., Zhao, li.(2020). Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. The Lancet, 395(10.1016), pp.S0140-6736.
- Peeri, N.C., Shrestha, N., Rahman, M.S., Zaki, R., Tan, Z., Bibi, S., Baghbanzadeh, M., Aghamohammadi, N., Zhang, W. and Haque, U., 2020. The SARS, MERS and novel coronavirus (COVID-19) epidemics, the newest and biggest global health threats: what lessons have we learned?. International journal of epidemiology, 49(3), pp.717-726.
- Ramadan, N. and Shaib, H., 2019. Middle East respiratory syndrome coronavirus (MERS-CoV): A review. Germs, 9(1), p.35.
- Rhodes, A., Evans, L.E., Alhazzani, W., Levy, M.M., Antonelli, M., Ferrer, R., Kumar, A., Sevransky, J.E., Sprung, C.L., Nunnally, M.E. and Rochwerg, B., 2017. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive care medicine, 43(3), pp.304-377.
- Røsjø, H., Varpula, M., Hagve, T.A., Karlsson, S., Ruokonen, E., Pettilä, V. and Omland, T., 2011. Circulating high sensitivity troponin T in severe sepsis and septic shock: distribution, associated factors, and relation to outcome. Intensive care medicine, 37(1), pp.77-85.
- Salata, C., Calistri, A., Parolin, C. and Palu, G., 2019. Coronaviruses: a paradigm of new emerging zoonotic diseases. Pathogens and disease, 77(9), p.ftaa006.
- Schultz, M.J., Dunser, M.W., Dondorp, A.M., Adhikari, N.K., Iyer, S., Kwizera, A., Lubell, Y., Papali, A., Pisani, L., Riviello, B.D. and Angus, D.C., 2017. Current challenges in the management of sepsis in ICUs in resource-poor settings and suggestions for the future. Intensive care medicine, 43(5), pp.612-624.
- Schwegmann-Wessels, C. and Herrler, G., 2006. Transmissible gastroenteritis virus infection: a vanishing specter. DTW. Deutsche tierarztliche Wochenschrift, 113(4), pp.157-159.
- Shang, W., Yang, Y., Rao, Y. and Rao, X., 2020. The outbreak of SARS-CoV-2 pneumonia calls for viral vaccines. npj Vaccines, 5(1), pp.1-3.
- Shi, J., Wen, Z., Zhong, G., Yang, H., Wang, C., Huang, B., Liu, R., He, X., Shuai, L., Sun, Z. and Zhao, Y., 2020. Susceptibility of ferrets, cats, dogs, and other domesticated animals to SARS–coronavirus 2. Science, 368(6494), pp.1016-1020.
- Sohrabi, C., Alsafi, Z., O’Neill, N., Khan, M., Kerwan, A., Al-Jabir, A., Iosifidis, C. and Agha, R., 2020. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19). International journal of surgery, 76, pp.71-76.
- The Harvard Gazette, Coronavirus Cases Hit 17,400 and Are Likely to Surge, (2020)
https://news.harvard.edu/gazette/story/2020/02/as-confirmed-cases-ofcoronavirus-surge-path-grows-uncertain/ - Tiwari, R., Dhama, K., Sharun, K., Iqbal Yatoo, M., Malik, Y.S., Singh, R., Michalak, I., Sah, R., Bonilla-Aldana, D.K. and Rodriguez-Morales, A.J., 2020. COVID-19: animals, veterinary and zoonotic links. Veterinary Quarterly, 40(1), pp.169-182.
- Wang, X.F., Yuan, J., Zheng, Y.J., Chen, J., Bao, Y.M., Wang, Y.R., Wang, L.F., Li, H., Zeng, J.X., Zhang, Y.H. and Liu, Y.X., 2020. Retracted: Clinical and epidemiological characteristics of 34 children with 2019 novel coronavirus infection in Shenzhen. Zhonghua er ke za zhi= Chinese journal of pediatrics, 58, pp.E008-E008.
- Wang, X.F., Yuan, J., Zheng, Y.J., Chen, J., Bao, Y.M., Wang, Y.R., Wang, L.F., Li, H., Zeng, J.X., Zhang, Y.H. and Liu, Y.X., 2020. Retracted: Clinical and epidemiological characteristics of 34 children with 2019 novel coronavirus infection in Shenzhen. Zhonghua er ke za zhi= Chinese journal of pediatrics, 58, pp.E008-E008.
- West, D. and Lansang, C., 2018. Global manufacturing scorecard: How the US compares to 18 other nations. Brookings, July, 10.
- World Health Organization, 2020. Coronavirus disease 2019 (COVID-19): situation report, 82.
- Xiao, K., Zhai, J., Feng, Y., Zhou, N., Zhang, X., Zou, J.J., Li, N., Guo, Y., Li, X., Shen, X. and Zhang, Z., 2020. Isolation and characterization of 2019-nCoV-like coronavirus from Malayan pangolins. BioRxiv.
- Yamamoto, V., Bolanos, J.F., Fiallos, J., Strand, S.E., Morris, K., Shahrokhinia, S., Cushing, T.R., Hopp, L., Tiwari, A., Hariri, R. and Sokolov, R., 2020. COVID-19: review of a 21st century pandemic from etiology to neuro-psychiatric implications. Journal of Alzheimer’s Disease, (Preprint), pp.1-45.
- Zhu, N., Zhang, D., Wang, W., Li, X., Yang, B., Song, J., Zhao, X., Huang, B., Shi, W., Lu, R. and Niu, P., 2020. A novel coronavirus from patients with pneumonia in China, 2019. New England journal of medicine.










Be the first to comment